IPTA Newsletter - October 2020

Presidential Message
 Dear All
Dear All
It is with sadness that I share the news that our first IPTA president John Najarian has died. We would like to celebrate his life and the difference he made to pediatric transplantation and send condolences to his family and colleagues (see his obituary – R. Fine). A really amazing man!
I trust you are all getting used to the new ‘normal’ and have all started your transplant programs again in those centres that stopped transplantation during the COVID pandemic. In South Africa, we are just emerging from a very tight 6-month lockdown this week, but watch the second wave in the Northern Hemisphere with a sense of despair – we really need a vaccine!
On the positive front, we have appointed our new committee members and it is great to have new ideas as the committee teams are already hard at work.
Our next highlights are the appointment of new candidates for Councilors and Officers positions beginning May 2021 and urge those interested in serving IPTA and the pediatric transplant community to apply before 30 November 2020.
We have just attended the TTS 2020 Virtual Congress which had an exciting separate pediatric track organized by Catherin Parker and Lars Pape with help from Katherine Twombley and Jonathan Johnson. This first of its kind meeting for TTS was entirely virtual and across 3 time zones - Montreal, Frankfurt and Seoul - enabling people from all over the world to participate (see our update from Gabriel Gondolesi).
We watched this congress with interest as we continue to plan our own Congress IPTA 2021, Prague Sept 11-14 and are still hoping to have a live meeting at least in some format. People enjoyed the TTS2020 congress but all agreed at a virtual networking event, that nothing quite beats drinking a Czech beer or Becherovka liquor in person with colleagues!
We also congratulate Marcelo Cantarovich on being elected TTS President as he takes over from Mehmet Haberal, and look forward to working with him.
Our Allied Health Professionals committee has changed their name to Allied Health and Nursing Professionals (AHNP) Committee and they have provided a charming story about Camp Chihopi. Please look out for their professional practice survey.
Our ‘Meet the Greats’ include Richard Trompeter and Steven Webber as pioneers in our field.
Our Pediatric Transplantation Journal (PETR) has had a great year with the impact factor once again increasing to 1.425 – congratulations to the editors and all those who participate with manuscripts as well as reviewing.
Look out for our Literary Review from the IPTA Education Committee and our Mentoring initiative.
We have started an international initiative around Advocacy for Children in Organ Allocation led by Evelyn Hsu, Stephen Marks and myself and would really appreciate a few minutes of your time answering a survey as we gather information about Pediatric Transplantation around the world.
Stay safe and thanks for all you do for the pediatric transplant community.
Best wishes
Mignon McCulloch
IPTA President
IPTA 2020

Do you wish to serve IPTA and the global pediatric transplant community? Or do you know someone who you believe is a pioneer in the field? The IPTA Nominations Committee is seeking qualified candidates to be considered for open Councilor and Officer positions beginning in May 2021.
All applications will be reviewed by the IPTA Nominations Committee, who will present a final slate of candidate Councilors and Officers to the IPTA membership for the 2021 election.
The IPTA Nominations Committee welcomes nominations and applications from anyone who has been an IPTA member in good standing for at least 1 year. Service to IPTA on committees or special activities relevant to the society is an asset.
The deadline for online submission of applications is November 30, 2020.
Application Procedure
Applications for open Councilor and Officer positions must be submitted using the online Call for Nominations Application. Completed applications must be submitted by November 30, 2020.
You will need the following before proceeding to the application:
- Briefly describe your role as it relates to pediatric transplantation (Limit 50 words)
- Please list any involvement or activities you have participated in with IPTA
- Briefly describe your reason for applying for a leadership position at this time (Limit 100 words)
- Nominee Statement (300 words): Identify and describe a key issue addressing a challenge in pediatric transplantation and why you believe that it is an important issue for IPTA to address. Please note that this will be used in materials sent to the IPTA membership.
To be uploaded on the site (pdf or Word documents):
- Two letters of support from two members in good standing of IPTA.
- Curriculum Vitae
Applicants will be notified in December 2020 as to the status of their acceptance to the slate of Councilors and Officers for the 2021 election.
Case Study


Virtual S’mores: Camp Chihopi in the Time of COVID
For many children, summer includes days at the pool, playing with friends, special vacations and maybe attending summer camp - a rite of passage for many. Being away from home, meeting new friends, and participating in activities leads to the development of new skills and greater independence. Some may think these experiences are unrealistic for children who are transplant recipients, but Camp Chihopi, created in 1995, has made that dream a reality. This annual event, through the Department of Transplant Surgery at UPMC Children’s Hospital of Pittsburgh, provides a non-medical environment that encourages campers to engage with peers of similar medical experiences within the setting of a summer camp. Chihopi provides an invaluable experience for young transplant recipients to learn skills to increase independence, build relationships with peers, improve self-esteem, and enhance understanding of their health, while participating in typical summer camp activities.
The summer of 2020 was going to be like the previous 25 summers – fun events, new and sustained friendships, making memories and being active in a beautiful camp setting. Then life changed dramatically for all with the COVID pandemic. Now what?
Faced with cancellations in every type of social encounter, it became evident that the safest plan was to cancel Chihopi 2020. Although we were becoming accustomed to cancellations, social distancing, masks, and virtual programming for school, meetings, and gathering with friends, it was still heartbreaking to cancel Chihopi. We had been hopeful that late summer might bring some normalcy, but adhering to current safety guidelines would be challenging with a camp environment that includes cabins of up to 12 campers and staff, a shared dining room, and close contact during activities. Following meetings with the Heart Camp leaders at Children’s Hospital, who were also planning a virtual camp, and internet research on other summer camps that were changing to a virtual platform, the Chihopi team began developing “V-CHOPI,” a virtual way to celebrate our friendships, connections, fun activities, and the spirit of Chihopi. About half of the usual group, 42 campers and 20 staff, participated in the week-long event.
Campers were invited to attend a 5-day event with specific programming that would take a virtual twist on favorite activities. Sitting around a campfire together and making S’mores wasn’t possible, but everyone could make their own campfires (cardboard paper towel rolls and colored tissue paper) and enjoy pre-made S’mores. Water sports weren’t available, but “Floatie Friday“ provided a challenge to present their unique version of a water activity – which could be swimming in the bathtub with flippers and a snorkel! The campers’ creativity, imagination and enthusiasm were amazing! With current events in mind, the theme of camp was “Mask-erade.” Each morning, campers received an email with instructions that included their thoughts about the question for the day, pictures to post related to the theme of the day, and preparation for activities. The week before camp, campers received the Chihopi Camp Cube by snail mail with supplies, a camp T-shirt, and other camp necessities. Two one-hour sessions, as recommended by national on-line camps, were scheduled and organized through Zoom. There were all-camp activities but campers were also divided into cabin groups for the afternoon session. Chihopi staff, including older transplant recipients and transplant team members, were also recruited and participated as session leaders.
V-Chihopi far exceeded our hopes for the event. We knew that campers would enjoy seeing each other, even virtually, and renewing friendships, but the strong connections, and the degree of openness and communication that occurred was unexpected. Each session had adult leadership from experienced camp staff and also one to two senior leaders to help facilitate discussions as needed. During activity sessions, campers would speak spontaneously about their medical experiences, peers, family and activities. One young camper remarked how his house “exploded” with alarms twice daily when it was time to take his medicine. This led to a long discussion about remembering to take medications and what strategies are used in their homes. In addition to taking meds, another theme was the bond they shared with other campers because of their transplant surgery. The campers discussed medical experiences from difficult times in the hospital to favorite nurses and tips in taking medicine that tasted “nasty.” Listening to campers, and the staff who are transplant recipients, discuss shared experiences and the support they receive from each other validated this virtual experience. In some ways, the virtual format seemed to encourage more personal discussion. Campers also enjoyed getting to know each other better through the backdrop of the campers’ homes. They could meet siblings, were introduced to pets (including a pot belly pig that could do tricks on demand!), saw stuffed animal collections and participated in a back-yard birthday party. Chihopi had an international perspective with our camp friends from the School of Nursing at Keio University in Tokyo who facilitated an origami session. The students and their instructor were active participants during camp week, despite the 13 hour time difference! “Ask the Transplant Team” was a fast hour of Q&A between the campers and team with insightful questions about transplant surgery to favorite ways to relax. Interestingly, the virtual format provided the ideal platform for this session, which had never been as successful at camp. With Zoom, the session became a more private interview and encouraged more discussion, positive exchange between campers and the team, and contributed to our understanding of each other because of our relationship through transplant.
This has been unforgettable summer in many ways. Although being together at Chihopi is what all the campers and staff hope for, it has become an opportunity to develop Chihopi as a virtual touchpoint throughout the year. Plans are being made for a holiday event, a planning session in the spring to engage the campers and staff for Chihopi 2021, and a virtual cabin orientation prior to camp. Rather than being only a place holder for “real” camp, V-Chopi strengthened the camp bond and is yet another experience the campers will have in common. Chihopi campers know that there are others with the same experiences and with whom they always have support and understanding. We learned that both virtual and real connections can be impactful.
Beverly Kosmach-Park
Director, Camp Chihopi
Publications Committee

The IPTA Publications committee would like to reach out to IPTA members to support our activity in encouraging mentorship for more junior colleagues.
Publishing is often difficult for less experienced researchers, especially for those who work in structures where performing research and writing of publications are not considered a priority.
The International Pediatric Transplant Association (IPTA) promotes the involvement of junior career members into the scientific community. For this reason, IPTA would like to facilitate the access to research projects and publication by initializing a mentorship program.
IPTA would like advanced clinician and researchers to consider becoming a mentor. We would like to propose different levels of mentorship, which one could engage in with a more junior colleague:
- The basic level of mentorship would be providing help with publication to non-native English speaker. The mentor will serve mainly as “proof reader”, i.e. will help with language corrections. Such help should not imply a substantial manuscript revision, therefore the mentor should not expect to share authorship of the paper and should only be acknowledged for her/his contribution
- The second option is that the mentor substantially contributes to the writing of the manuscript. As this is more demanding a shared authorship may be discussed with the mentee and her/his institution depending on the extent of the contribution.
- A third level of mentorship would involve the mentor already during project design and research development. At this higher level of mentorship, the mentor may also give advice to professional development of her/his mentee. In case this contribution should lead to publication, we would strongly advice that authorship should be shared
- In specific cases, mentorship could be an ongoing process, which could lead to a “visiting professorship” of the respective mentor at the mentee’s institution. This could include an active engagement of the mentor by providing educational webinars on e.g. “Manuscript writing”, “Designing and developing a research project”.
We are aware that the level of involvement may change over time and should be adjusted by mutual understanding between mentor and mentee to reach their expectations.
We would appreciate if senior IPTA members would be willing to provide mentorship at one of the levels indicated. Once you indicated your willingness to support the program, we would list your name, area of expertise and level of engagement you are willing to provide on IPTA’s website. If there are any further questions, please contact Anette Melk (melk.anette@mh-hannover.de).
Advocacy for Children in Organ Allocation

The International Pediatric Transplant Association believes that it is important to represent the international community of members and the patients and the families they serve. By broadening our reach into advocacy, we can advance the cause of children and youth who stand to benefit from transplantation worldwide.
The International Advocacy group has the intention to survey the existing landscape of allocation for pediatric transplantation, define an ethical mandate for pediatric priority in deceased donor allocation to pediatric recipients, and determine an optimal path forward to execute this mandate on an international scale.
Please respond to this survey link in order to provide information to help us define allocation practices for children worldwide! Thank you for your care of children and your involvement in the IPTA.
Meet the Greats!

 Richard Trompeter, UK
Richard Trompeter, UK
Dr. Richard Trompeter is Emeritus Consultant Paediatric Nephrologist at Great Ormond Street Hospital for Children (GOSH), London, and Honorary Consultant Nephrologist and Clinical Academic at University College London Centre for Nephrology, The Royal Free Hospital. He is a graduate of Guy’s Hospital School of Medicine, London.
He trained in paediatric nephrology at GOSH and the Institute of Child Health where as a research fellow he developed an interest in nephrotic syndrome, which remains a major clinical and academic part of his career. He completed his training at Guy’s where between 1979 -1983 and was privileged to be part of the team responsible for pioneering kidney transplantation in some of the youngest children in the UK at that time.
He was appointed as Consultant Paediatric Nephrologist at The Royal Free Hospital in 1984 and set up the renal transplant programme for children in the north of London and subsequently established the dialysis and kidney transplant programme for children at GOSH in 1986, and became a full time Consultant at GOSH in 1989. The transplant service developed a national and international reputation, and he was a major participant in initial randomised clinical trials to demonstrate efficacy of various immunosuppressive regimens.
He was appointed the first Chairman of the GOSH Clinical Ethics Committee in 2000.
He retired from GOSH in 2009 and set up the first Transition Service for young adults with CKD at the UCL Centre for Nephrology at The Royal Free Hospital campus. Current research is focused on the molecular genetics of nephrotic syndrome and the benefit of transition services.
He has been a supporter of IPTA from 2005, serving on many committees, Council and EC. President from 2013 – 2015 and founding Chairman of the Ethics Committee 2017 -2019.
He is a past President of the Paediatric and Child Health Section of the Royal Society of Medicine, and previously a member of the Ethics Committees of the British Transplant Society, European Renal Association and TTS.
Married to Babs, they have four children, Sara a Consultant Haematologist, Alex a Consultant Orthopaedic Surgeon, Nick a Barrister, Becky the marketing and production manager for the National Society for the Prevention of Cruelty to Children (NSPCC), and eight grandchildren.
 Steven Webber, USA
Steven Webber, USA
Dr. Steven Webber is the Chair of the Department of Pediatrics at Vanderbilt University and the James C. Overall Professor of Pediatrics. He also serves as Pediatrician-in-Chief of the Monroe Carell Jr. Children’s Hospital. He is a native of the UK and graduated from the University of Bristol Medical School. He trained in internal medicine, pediatrics and pediatric cardiology in the UK, Canada and the US. He joined the faculty of the Children’s Hospital / University of Pittsburgh in 1994 where he served as Chief of the Division of Pediatric Cardiology, Co-Director of the Heart Institute, and Medical Director of the Heart and Heart-Lung Transplantation Program.
His research interests include post-transplant lymphoproliferative disorders, understanding the genetic contributions to graft and patient outcomes and the role of antibodies in determining graft outcomes after pediatric thoracic transplantation. Dr. Webber has been the recipient of numerous federal and foundation grants. He has published widely and is the author of over 200 peer-reviewed publications. He has served as the Editor-in-Chief of the journal Pediatric Transplantation and is Co-Editor of three textbooks: Pediatric Solid Organ Transplantation, Post-Transplant Lymphoproliferative Disorders and Textbook of Organ Transplantation.
Dr. Webber has served as President of both the International Pediatric Transplant Association (IPTA) and the Pediatric Heart Transplant Study. He is a past Chair of the Thoracic Committee of the United Network for Organ Sharing. He has served on the Board of Directors of the American Society of Transplantation and of the International Society for Heart and Lung Transplantation. He recently received the 2019 IPTA Pioneer Award.
He enjoys reading history and learning Norwegian.
Survey

Dear Transplant Colleagues,
The IPTA Allied Health and Nursing Professionals (AHNP) committee have compiled a professional practice survey.
The goals of this survey are:
- To describe the prevalence and diversity of the clinical, research and teaching practice of Allied Health (AH) and Nursing team members internationally.
- To understand the multidisciplinary composition of transplant care teams and develop an international framework regarding professional practice.
- To identify possible barriers and challenges for AH and Nursing professionals within their role, with the aim of improving and supporting AH and Nursing practice development specifically within the field of pediatric transplant.
- To support a publication related to international AH and Nursing practice in pediatric solid organ transplantation
If you are an Allied Health or Nursing professional (both members and non-members of IPTA): please consider completing the survey (see link below) and forwarding it to your non-IPTA colleagues.
Physicians and other members: Please share this email with your Allied Health and Nursing colleagues at your centre, and encourage them to complete the survey (You do not have to be a member of IPTA to complete this survey)
You may open the survey in your web browser by clicking the button below.
IPTA Allied Health and Nursing Survey
The survey should only take about 5-10 minutes to complete. You participation is voluntary, and all responses will be de-identified to ensure anonymity.
We are extremely grateful for your time
IPTA AHNP Committee
IPTA 2021
In Memoriam
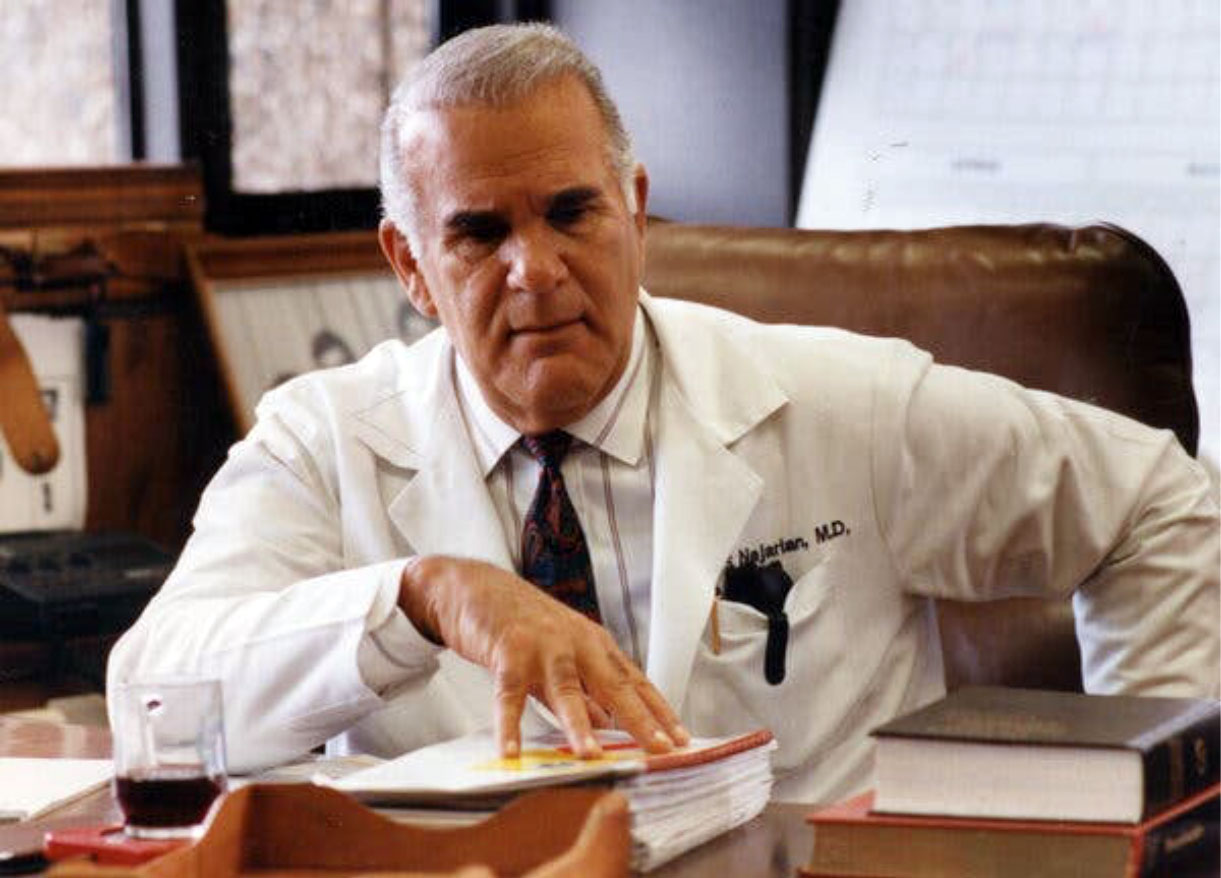
It is with deep sadness that the members of IPTA mourn our first President (2001-2003) John S. Najarian.
After completing his surgical training John joined the faculty at the University of California San Francisco and initiated one of the first kidney transplant programs in the United States which included transplanting children. In 1967 John moved to the University of Minnesota to head the Department of Surgery, a position he held until 1993.
John was physically a “big” man but one of his passions was transplanting infants and young small children with End Stage Kidney Disease. The group at Minnesota led the way in demonstrating the ability to overcome the technical abilities in transplanting kidneys from either live-related or deceased donors into infants.
John organized the first international meeting on organ transplantation in children in in 1995 in Minneapolis. It was a huge success and led to a second meeting in Paris in 1997 at which time the ground work for the Journal Pediatric Transplantation was initiated. The inaugural meeting of IPTA took place in Venice, Italy in 1999 at which time the by-laws of IPTA were developed and Dr Najarian was identified for a leadership role in the nascent organization. The next meeting under John’s leadership was to take place in Rio de Janeiro Brazil in 2001; but the catastrophe of the Twin Towers in New York City dictated a delay of one year. John guided to organization during this very difficult time and ultimately was the first President of an IPTA Congress in Rio in 2002.
Dr Najarian was not only a superb transplant surgeon but also an excellent scientist.
IPTA membership is deeply saddened by Dr Najarian’s passing and we send our heartfelt condolences to the members of his family.
Richard N. Fine, MD
Distinguished Professor of Pediatrics
Renaissance School of Medicine at Stony Brook University
Stony Brook NY, USA
Past President and Secretary – Treasurer of IPTA
Literary Review

Literary review provided by Rupesh Raina, MD on behalf of the IPTA Education Committee.
Pediatric Transplantation and COVID-19
30.6 million COVID-19 cases, 950,000 deaths, an increase of two million cases in the third week of September accompanied the new record number of reported cases of COVID-19 in a single week.1 Despite increased awareness and dedication to understanding the effect of the virus, there are gaps in the knowledge that affect the management of children, especially those undergoing transplantation procedures. Coupled with the emergence of novel and existing strains that disproportionally affect children and immunocompromised, there remain concerns COVID-19 strains may further complicate treatment after transplant.2,3,4 Although respiratory viral infections can occur in up to 38% of patients following transplant and follow-up has reduced mortality to below 4%, known poor outcomes among the immunocompromised with COVID-19 necessitate definite consensus.5,6
Ongoing discussion on epidemiology has established that illness among pediatric patients is frequently asymptomatic and, if not, presents with mild to moderate severity.8,9,10 It is noted that the pediatric patients present with lower rates of fever, cough, shortness of breath, and require less hospitalization than counterpart cohorts in the age range between 16 and 64.11,12 This finding mirrors the predicated results from prior outbreaks with the SARS and MERS associated coronaviruses.13,14 There are still cases of critically ill pediatric patients with COVID-19; case reports spanning the international community highlight complications of pediatric patients with comorbidities alongside shock and multisystem inflammation post-infection.15,16,17,18
There remain major gaps in establishing the differing prognosis of disease in children compared to adults. Reviews of cases reflect little discrepancy in transmission and infection rate compared to the adult population although most noted clinical risk score calculators (including COVID-GRAM) place emphasis on age. 19,20,21 Potential explanations for disease progression in pediatric population ranges from specific concentrations of angiotensin-converting enzymes (brought to attention by effect of ACEIs), humoral immunity response via interferons, cathepsin activity, and altered T-cell response due to age.21,22,23 Adding to the murkiness of the impact of COVID-19 on pediatric transplant populations, there is no consensus on the effect of immunosuppression particularly due to the potential therapeutic effects in managing observed cytokine storm in rare cases.24,25,26,27 Furthermore, though there are efforts underway to develop consensus statements for transplants in adult cases, there is an essential need for systematic data from pediatric settings to address consequences.28,29,30
The rapid transmission of COVID-19 has exposed the limited knowledge on the coronaviruses, particularly in children. The inadequate information for pathogenic differences in response to SARS-CoV-2 in pediatric cases and the immunocompromised has mystified the vital clinical management of immunosuppressed pediatric transplant patients. There are optimistic signs in initiating multi-center data collection to address these issues and preliminary data suggests prognoses of children receiving transplants may parallel immunocompetent children; however, further targeted and collaborative investigations are key to not only improving outcomes of COVID-19 in pediatric transplant cases but also in demystifying the viral pathological process.31
References
- WHO COVID-19 – Situation Report, 05/05/2020. 2020. at https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/
- Abdul-Rasool S, Fielding BC. Understanding Human Coronavirus HCoV-NL63. Open Virol J. 2010;4:76-84. Published 2010 May 25. doi:10.2174/1874357901004010076
- Kumar D, Michaels MG, Morris MI, Green M, Avery RK, Liu C, Danziger-Isakov L, Stosor V, Estabrook M, Gantt S, Marr KA, Martin S, Silveira FP, Razonable RR, Allen UD, Levi ME, Lyon GM, Bell LE, Huprikar S, Patel G, Gregg KS, Pursell K, Helmersen D, Julian KG, Shiley K, Bono B, Dharnidharka VR, Alavi G, Kalpoe JS, Shoham S, Reid GE, Humar A; American Society of Transplantation H1N1 Collaborative Study Group. Outcomes from pandemic influenza A H1N1 infection in recipients of solid-organ transplants: a multicentre cohort study. Lancet Infect Dis. 2010 Aug;10(8):521-6. doi: 10.1016/S1473-3099(10)70133-X. Epub 2010 Jul 9. PMID: 20620116; PMCID: PMC3045703.
- Choi SM, Boudreault AA, Xie H, Englund JA, Corey L, Boeckh M. Differences in clinical outcomes after 2009 influenza A/H1N1 and seasonal influenza among hematopoietic cell transplant recipients. Blood. 2011 May 12;117(19):5050-6. doi: 10.1182/blood-2010-11-319186. Epub 2011 Mar 3. PMID: 21372154; PMCID: PMC3109531.
- Tsoumakas K, Giamaiou K, Goussetis E, Graphakos S, Kossyvakis A, Horefti E, Mentis A, Elefsiniotis I, Pavlopoulou ID. Epidemiology of viral infections among children undergoing hematopoietic stem cell transplant: Α prospective single-center study. Transpl Infect Dis. 2019 Aug;21(4):e13095. doi: 10.1111/tid.13095. Epub 2019 May 2. PMID: 30993823.
- Danziger-Isakov L, Steinbach WJ, Paulsen G, et al. A Multicenter Consortium to Define the Epidemiology and Outcomes of Pediatric Solid Organ Transplant Recipients With Inpatient Respiratory Virus Infection. J Pediatric Infect Dis Soc. 2019;8(3):197-204. doi:10.1093/jpids/piy024
- Eastin C, Eastin T. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China: Dong Y, Mo X, Hu Y, et al. Pediatrics. 2020; doi: 10.1542/peds.2020-0702. J Emerg Med. 2020;58(4):712-713. doi:10.1016/j.jemermed.2020.04.006
- Jutzeler CR, Bourguignon L, Weis CV, Tong B, Wong C, Rieck B, Pargger H, Tschudin-Sutter S, Egli A, Borgwardt K, Walter M. Comorbidities, clinical signs and symptoms, laboratory findings, imaging features, treatment strategies, and outcomes in adult and pediatric patients with COVID-19: A systematic review and meta-analysis. Travel Med Infect Dis. 2020 Aug 4;37:101825. doi: 10.1016/j.tmaid.2020.101825. Epub ahead of print. PMID: 32763496; PMCID: PMC7402237.
- Foust AM, McAdam AJ, Chu WC, Garcia-Peña P, Phillips GS, Plut D, Lee EY. Practical guide for pediatric pulmonologists on imaging management of pediatric patients with COVID-19. Pediatr Pulmonol. 2020 May 28:10.1002/ppul.24870. doi: 10.1002/ppul.24870. Epub ahead of print. PMID: 32462724; PMCID: PMC7283678.
- Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, et al. . Epidemiological characteristics of 2143. pediatric patients with 2019 coronavirus disease in China. Pediatrics. (2020). e20200702. 10.1542/peds.2020-0702
- CDC COVID-19 Response Team. Coronavirus Disease 2019 in Children - United States, February 12-April 2, 2020. MMWR Morb Mortal Wkly Rep. 2020 Apr 10;69(14):422-426. doi: 10.15585/mmwr.mm6914e4. PMID: 32271728; PMCID: PMC7147903.
- Dong, Yuanyuan, Xi Mo, Yabin Hu, Xin Qi, Fang Jiang, Zhongyi Jiang, and Shilu Tong. "Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China." Pediatrics (2020).
- Al-Tawfiq JA, Kattan RF, Memish ZA. Middle East respiratory syndrome coronavirus disease is rare in children: An update from Saudi Arabia. World J Clin Pediatr. 2016;5(4):391-396. Published 2016 Nov 8. doi:10.5409/wjcp.v5.i4.391
- Stockman LJ, Massoudi MS, Helfand R, et al. Severe acute respiratory syndrome in children. Pediatr Infect Dis J. 2007;26(1):68-74. doi:10.1097/01.inf.0000247136.28950.41
- Patel PA, Chandrakasan S, Mickells GE, Yildirim I, Kao CM, Bennett CM. Severe Pediatric COVID-19 Presenting With Respiratory Failure and Severe Thrombocytopenia. Pediatrics. 2020;146(1):e20201437. doi:10.1542/peds.2020-1437
- André N, Rouger-Gaudichon J, Brethon B, et al. COVID-19 in pediatric oncology from French pediatric oncology and hematology centers: High risk of severe forms?. Pediatr Blood Cancer. 2020;67(7):e28392. doi:10.1002/pbc.28392
- Nguyen DC, Haydar H, Pace ER, Zhang XS, Dobbs KR. Pediatric Case of Severe COVID-19 With Shock and Multisystem Inflammation. Cureus. 2020 Jun 29;12(6):e8915. doi: 10.7759/cureus.8915. PMID: 32742881; PMCID: PMC7389873.
- Sun, D., Li, H., Lu, X. et al. Clinical features of severe pediatric patients with coronavirus disease 2019 in Wuhan: a single center’s observational study. World J Pediatr 16, 251–259 (2020). https://doi.org/10.1007/s12519-020-00354-4
- Rajmil L. Role of children in the transmission of the COVID-19 pandemic: a rapid scoping review. BMJ Paediatr Open. 2020;4(1):e000722. Published 2020 Jun 21. doi:10.1136/bmjpo-2020-000722
- Liang W, Liang H, Ou L, et al. Development and Validation of a Clinical Risk Score to Predict the Occurrence of Critical Illness in Hospitalized Patients With COVID-19. JAMA Intern Med. 2020;180(8):1081-1089. doi:10.1001/jamainternmed.2020.2033
- Bellino S, Punzo O, Rota MC, Del Manso M, Urdiales AM, Andrianou X, Fabiani M, Boros S, Vescio F, Riccardo F, Bella A, Filia A, Rezza G, Villani A, Pezzotti P; COVID-19 Working Group. COVID-19 Disease Severity Risk Factors for Pediatric Patients in Italy. Pediatrics. 2020 Jul 14:e2020009399. doi: 10.1542/peds.2020-009399. Epub ahead of print. PMID: 32665373.
- European Centre for Disease Prevention and Control. 2020. COVID-19 In Children And The Role Of School Settings In COVID-19 Transmission. [online] Available at: <https://www.ecdc.europa.eu/en/publications-data/children-and-school-settings-covid-19-transmission> [Accessed 22 September 2020].
- South AM, Brady TM, Flynn JT. ACE2 (Angiotensin-Converting Enzyme 2), COVID-19, and ACE Inhibitor and Ang II (Angiotensin II) Receptor Blocker Use During the Pandemic: The Pediatric Perspective. Hypertension. 2020 Jul;76(1):16-22. doi: 10.1161/HYPERTENSIONAHA.120.15291. Epub 2020 May 5. PMID: 32367746; PMCID: PMC7289676.
- Zhang Y, Xu J, Jia R, Yi C, Gu W, Liu P, Dong X, Zhou H, Shang B, Cheng S, Sun X, Ye J, Li X, Zhang J, Ling Z, Ma L, Wu B, Zeng M, Zhou W, Sun B. Protective humoral immunity in SARS-CoV-2 infected pediatric patients. Cell Mol Immunol. 2020 Jul;17(7):768-770. doi: 10.1038/s41423-020-0438-3. Epub 2020 May 7. PMID: 32382126; PMCID: PMC7203722.
- Lai Q, Spoletini G, Bianco G, et al. SARS-CoV2 and immunosuppression: A double-edged sword [published online ahead of print, 2020 Jul 8]. Transpl Infect Dis. 2020;e13404. doi:10.1111/tid.13404
- Shivakumar S, Smibert OC, Trubiano JA, Frauman AG, Liew DF. Immunosuppression for COVID-19: repurposing medicines in a pandemic. Aust Prescr. 2020;43(4):106-107. doi:10.18773/austprescr.2020.037
- Mehta P, McAuley DF, Brown M, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033-1034. doi:10.1016/S0140-6736(20)30628-0
- Doná D, Torres Canizales J, Benetti E, Cananzi M, De Corti F, Calore E, Hierro L, Ramos Boluda E, Melgosa Hijosa M, Garcia Guereta L, Pérez Martínez A, Barrios M, Costa Reis P, Teixeira A, Lopes MF, Kaliciński P, Branchereau S, Boyer O, Debray D, Sciveres M, Wennberg L, Fischler B, Barany P, Baker A, Baumann U, Schwerk N, Nicastro E, Candusso M, Toporski J, Sokal E, Stephenne X, Lindemans C, Miglinas M, Rascon J, Jara P; ERN TransplantChild. Pediatric transplantation in Europe during the COVID-19 pandemic: Early impact on activity and healthcare. Clin Transplant. 2020 Aug 12:e14063. doi: 10.1111/ctr.14063. Epub ahead of print. PMID: 32786120; PMCID: PMC7435500.
- Al-Judaibi B, Almaghrabi R, Alghamdi M, Al-Hamoudi WK, AlQahtani M, Abaalkhail F, Shagrani M, Sanai FM. Saudi association for the study of liver diseases and transplantation position statement on liver transplantation during the COVID-19 pandemic. Saudi J Gastroenterol. 2020 Sep-Oct;26(5):233-239. doi: 10.4103/sjg.SJG_131_20. PMID: 32341229.
- Merhi B, Gohh R. Kidney Transplantation and COVID-19. R I Med J (2013). 2020 Sep 4;103(8):34-37. PMID: 32900010.
- Goss MB, Galván NTN, Ruan W, Munoz FM, Brewer ED, O'Mahony CA, Melicoff-Portillo E, Dreyer WJ, Miloh TA, Cigarroa FG, Ranch D, Yoeli D, Adams MA, Koohmaraie S, Harter DM, Rana A, Cotton RT, Carter B, Patel S, Moreno NF, Leung DH, Goss JA. The Pediatric Solid Organ Transplant Experience with COVID-19: An Initial Multi-Center, Multi-Organ Case Series. Pediatr Transplant. 2020 Sep 18:e13868. doi: 10.1111/petr.13868. Epub ahead of print. PMID: 32949098.
TTS 2020 Virtual Congress
This year the 28th International biennial Congress of The Transplantation Society was planned to take place in Seoul, Korea. However, unfortunately the Sars-Cov2 (COVID 19) pandemic forced us to change the format of the Congress to a Virtual event. The decision was not easy and the timing to change the format a real challenge, but the meeting was not cancelled, or postponed; it was held as planned, though virtually.
Today we are very pleased to inform you that from September 13 to 18th, we witnessed a transformative and successful meeting that was able to bring together experts from all the regions of the transplant world, to share under this new format their latest science and knowledge in the field of transplantation.
The congress showed a superb technological development and support, allowing 3,336 healthcare professionals from around the world to have immediate and simultaneous access to knowledge and interaction with colleagues and experts, by using 3 full programs per day to accommodate all the time zones.
A total of 1,105 abstracts were submitted. 31 State of the art conferences (including Pediatric Transplantation), 38 oral presentations, 21 E-Posters, 25 Workshops, 4 TID dedicated activities, 3 plenary sessions and 2 Covid and sponsored symposium as well the Awards session could be seen on line. All registrants will have access for one year to all recorded sessions using the virtual congress web app.
Click here for WebApp (virtual.tts.org)
A lot was learned by the Scientific Program Committee and by the TTS staff and leadership, who were able to adjust to the current reality, for the benefit of the whole transplant society.
At the end of the meeting and hoping to meet again in person, it was announced that the next meeting will be placed for the first time in Latin-América, (the region that counts the largest number of TTS members), and the selected city is Buenos Aires. Place a save-the-date for September 10-14th, 2022 and join us in the wonderful city of Buenos Aires.
Prof. Gabriel E. Gondolesi, MD
Former LA TTS Council
Current TTS Treasurer
Pediatric Transplantation

Submitted by Burkhard Tonshoff & Sharon Bartosh on behalf of Pediatric Journal of Transplantation.
Impact Factor
The 2019 Impact Factors (IF) for Pediatric Transplantation (PETR) was released some weeks ago: PETR saw another great year with the 2-year IF increasing to 1.425 (up from 1.326). This is a great success of the entire Editorial Team of PETR and our reviewers. Many thanks for your hard work and this excellent collaboration!
Editorial Board
The Editorial Board of PETR has recently been rejuvenated. We thank those colleagues who have retired for their previous hard work for the journal and welcome their successors: Associate Editor “Transplant Immunobiology”: Adriana Zeevi. Editorial Board “Kidney”: Bethany Foster, Montreal, Canada; Britta Höcker, Heidelberg, Germany; Joshua Kausman, Melbourne, Australia; Anette Melk, Hannover, Germany; Asha Moudgil, Washington, USA. “Liver”: Christine S. Hwang, Dallas, USA; Eirini Kyrana, Leeds, UK; Emily Perito, San Francisco, USA; James E Squires, Pittsburgh, USA; Gordon Thomas, Sydney, Australia; Nam-Joon Yi, Seoul, Korea. “Heart/Lung”: Justin Godown, Nashville, USA; Jeffrey Gossett, San Francisco, USA; Nicolaus Schwerk, Hannover, Germany; Brigitte Stiller, Freiburg (Bad Krozingen), Germany; Glen Philip Westall, Melbourne, Australia. “Intestine”: Yaron Avitzur, Toronto, Canada; Jonathan Hind, London, UK; Mureo Kasahara, Tokyo, Japan. “Stem Cell”: Behnam Sadeghi, Huddinge, Sweden; Jacek Toporski, Lund, Sweden. “Transplant Immunobiology”: Tom D. Blydt-Hansen, Vancouver, Canada; Eileen Chambers, Durham, USA; Michael Seifert, Birmingham, USA. “Infectious Diseases”: Sandra Asner, Lausanne, Switzerland; Daniel Dulek, Nashville, USA. “Quality of Life”: Anna Gold, Toronto, Canada; Nataliya Zelikovsky, Philadelphia, USA.
Special Sections/Issues
PETR is very much interested in publishing Special Sections or Issues with a series of review articles on a specific overarching topic. The April issue of PETR (volume 24, issue 3) published a series of articles as an “International Consensus Statement on Donor Management in Pediatric Heart Transplant” (Guest Editors Anne Dipchand and Richard Kirk). There is an upcoming special issue on the topic “Healthy Living in Pediatric Transplant Patients” (Guest Editors Asha Moudgil and Priya Verghese). If you have an idea on a Special Section/Issue of PETR on a cutting-edge topic and would like to act as the guest editor, please contact the Editors-in-Chief Sharon Bartosh and Burkhard Tönshoff.
Review articles
There is a recent initiative of the PETR Editorial Team on soliciting Review Articles for the journal from experts in the field. The Editors-in-Chief, the Deputy Editors and Associate Editors have identified several cutting-edge research topics or important clinical themes which require an update. Please contact us if you or your group is interested in joining us in this initiative.
Social Media
Thanks to our Associate Editor for Social Media Vikas R. Dharnidharka, our journal is now on Twitter, with 416 followers at the time of this writing! This allows the journal and individual authors to publicize their work. Our associated International Pediatric Transplant Association (IPTA) is now also on Twitter. We have now integrated into our manuscript submission system two questions about an author’s Twitter handle (if available), and if the author would be interested in participating in a Twitter journal club if their article is accepted (voluntary). We hope to have our first Twitter journal club soon.
Contact
Address
Cell Transplant and Regenerative Medicine Society
c/o The Transplantation Society
740 Notre-Dame Ouest
Suite 1245
Montréal, QC, H3C 3X6
Canada






