Welcome to the
International Society of Vascularized Composite Allotransplantation
ISVCA 2025 - NASEM Pre-recorded Presentations
You will recall that our congress program fell behind schedule on Sunday afternoon and our session on "Global Administrative Challenges in VCA" had to be cut short. The video presentations by Dr. Ken Kizer and Dr. Linda Cendales, which unfortunately could not be shown in Helsinki, are now accessible within the members area of the ISVCA website.
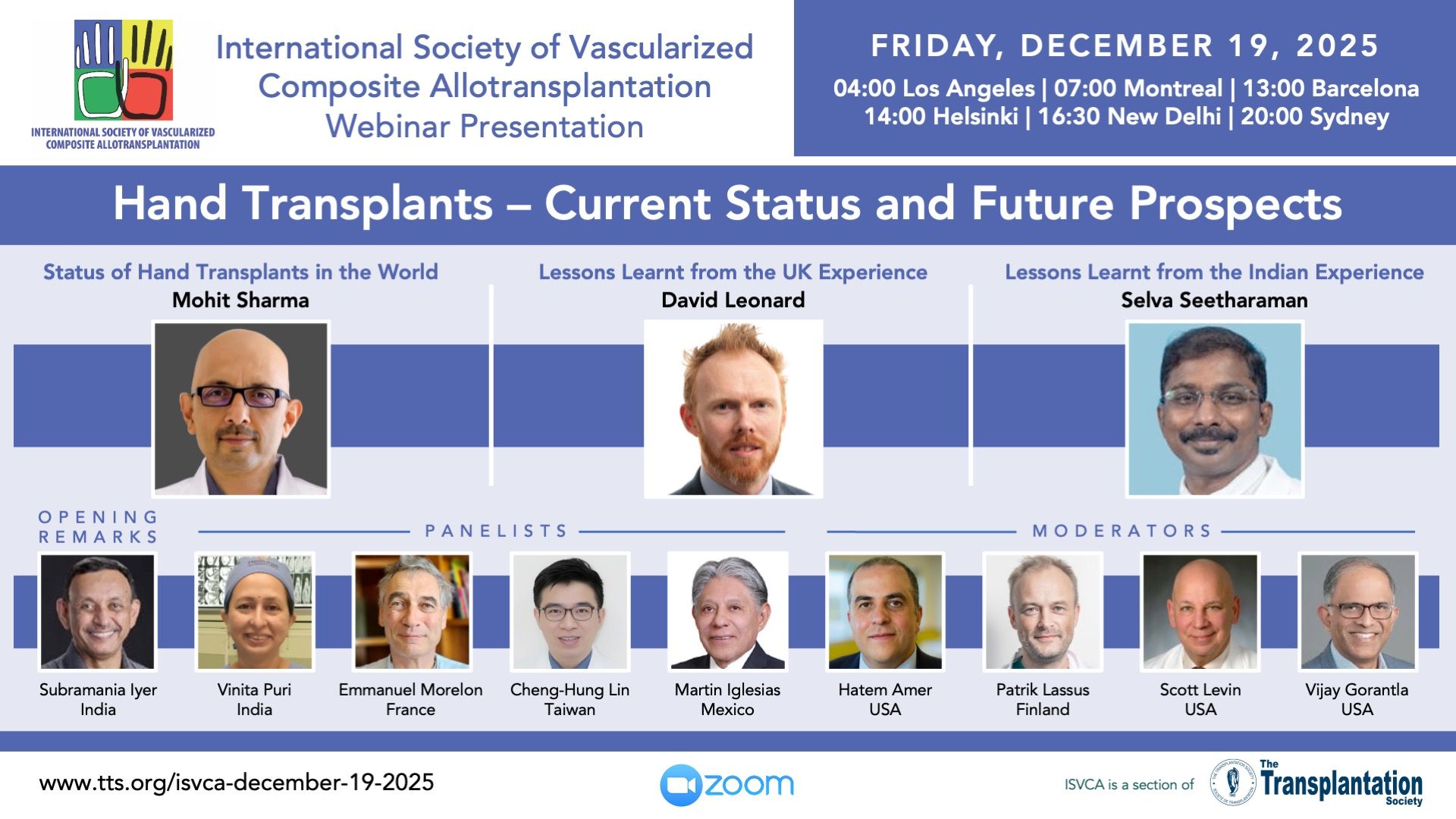
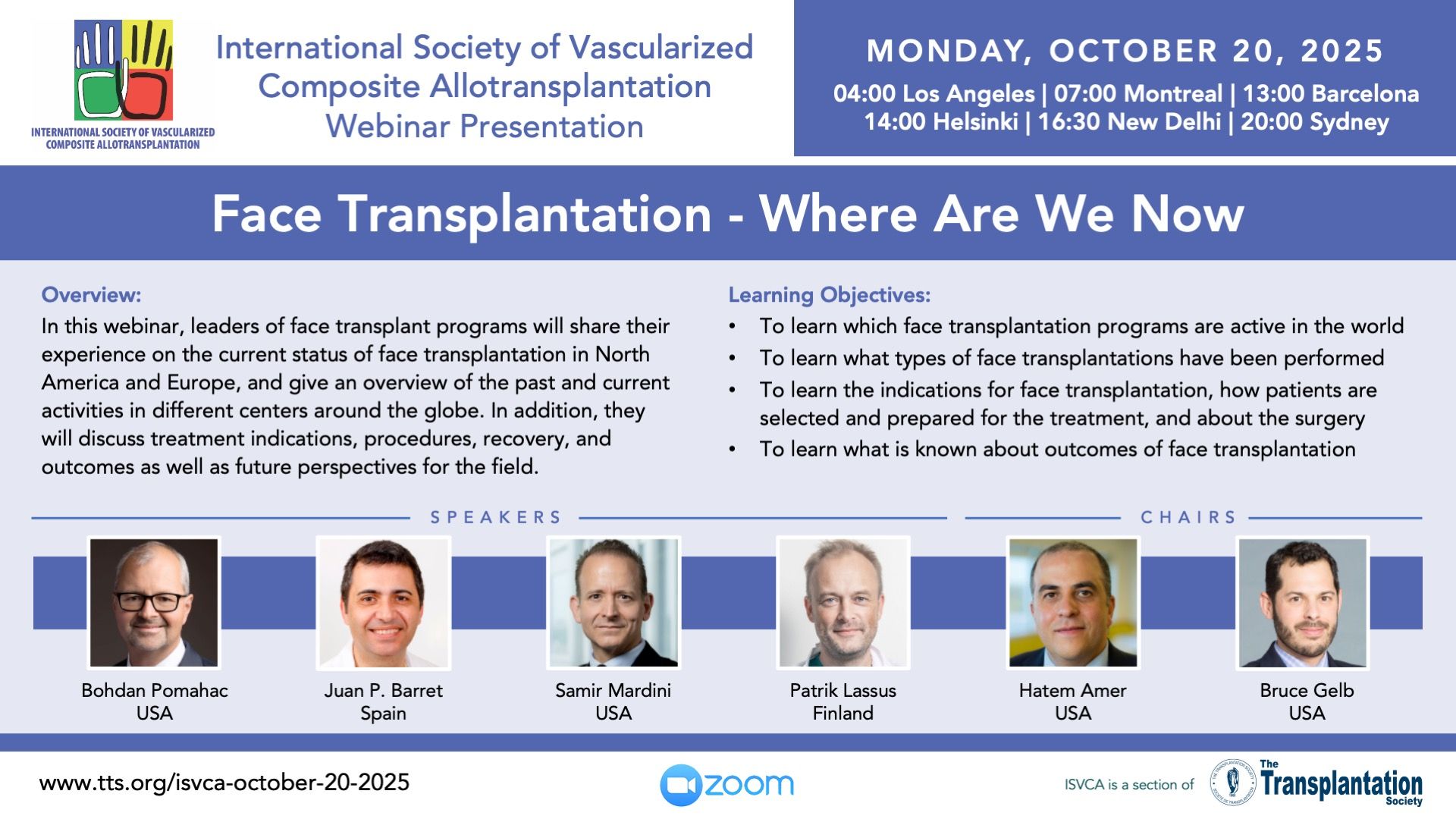
Recent Webinar Recordings

Official Journal of the
International Society of Vascularized Composite Allotransplantation
ISVCA Transplant Centers Map
Contact
Address
International Society of Vascularized Composite Allotransplantation
c/o The Transplantation Society
740 Notre-Dame Ouest
Suite 1245
Montréal, QC, H3C 3X6
Canada