About IPTA
Donate Today!
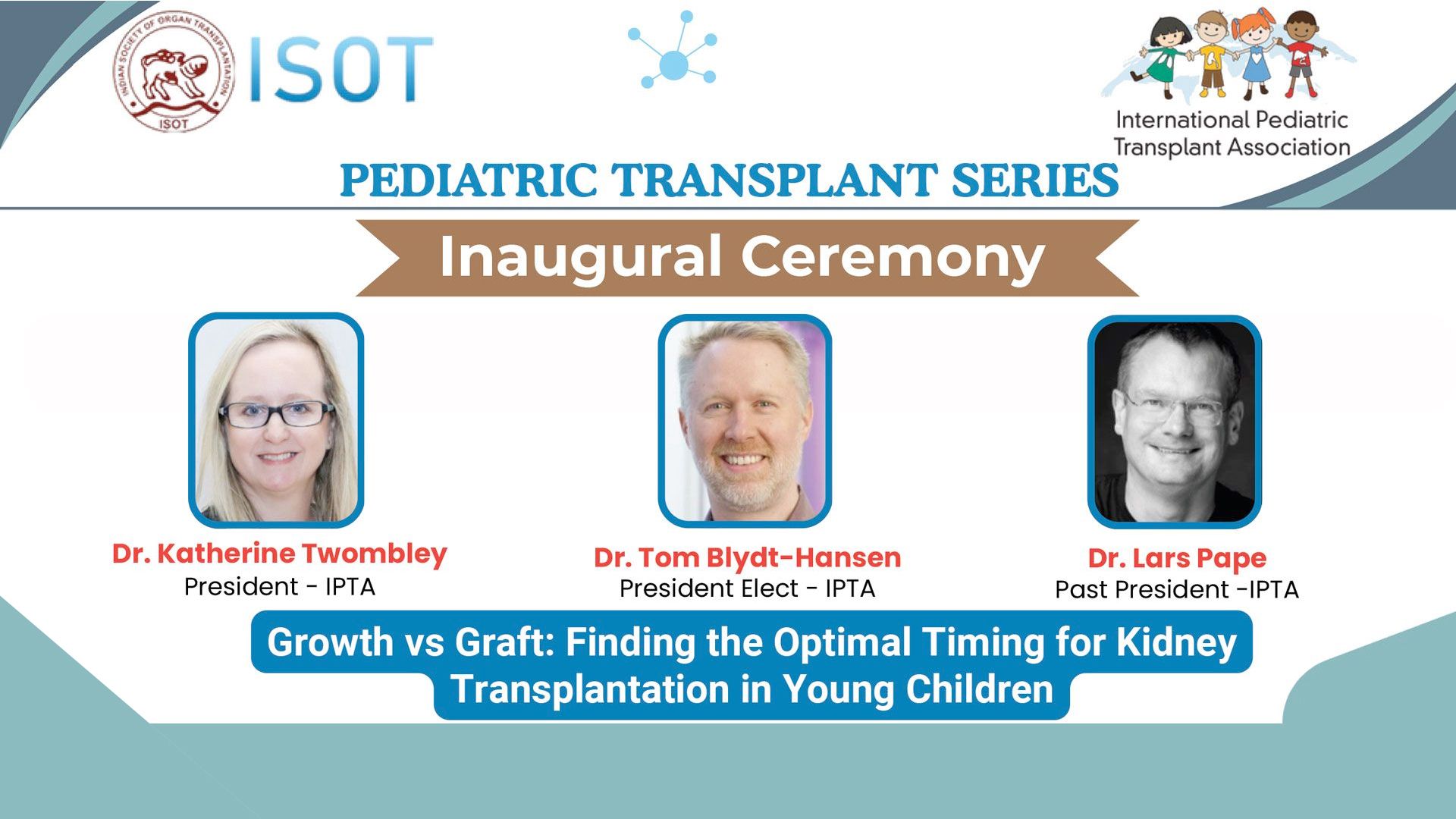
Upcoming IPTA-ISOT Presentation

The next webinar in our series will take place on Friday 20th March at 18:30pm IST (Indian Standard Time) and is entitled ‘Bladder and Lower Urinary Tract Optimization in Pediatric Kidney Transplantation’, presented by Dr. Andre Dick, Seattle Children's Hospital, USA; and Dr. Shreya Gawadem, Dr. D Y Patil Medical College Hospital and Research Centre, India. Opening remarks and case introduction by Dr. Lars Pape, IPTA Past-President.
Are You Interested in Joining an IPTA Committee?

Active members of the IPTA are integral in continuing to further our mission of advancing the science and practice of pediatric transplantation worldwide in order to improve the health of all children who require such treatment. Our committees are responsible for setting and working towards yearly goals and objectives that will positively contribute to knowledge sharing amongst our peers practicing in the field of pediatric transplantation. Committee members are appointed by the IPTA Council and are invited to serve 2-year terms effective May 2026.
Expressions of interest will be accepted from IPTA members until April 1, 2026. Please complete the interest form by clicking the button below.
Upcoming IPTA Communities Calls

IPTA has established organ-specific Communities forums (Liver, Thoracic and Kidney) providing our members an opportunity to contribute and enrich IPTA's activities. Organ-specific Communities are envisioned to spearhead guideline development, foster discussions on organ allocation, and delve into various specific other subjects. Visit the Communities page for details on our upcoming calls. (must be logged in to view)
The next calls will be Tuesday, February 24, 2026, 13:30pm EST (Liver Community); and Thursday, May 7, 2026, 12:00 EDT (Kidney Community).
Mentoring Program

TTS IPTA TID Position Statement on Vaccines in Transplant Recipients

Child Organ Allocation Advocacy: An International Initiative
The International Pediatric Transplant Association (IPTA) is dedicated to advocating for equitable access to life-saving transplants for children worldwide. Despite advancements in transplant medicine, disparities in organ allocation persist, with pediatric waitlist mortality remaining a critical challenge. Addressing this issue requires a global effort to understand current practices and identify areas for improvement.
The IPTA International Advocacy Group has developed a survey to gather insights on pediatric liver transplant allocation policies and programs worldwide. We have made organ-specific surveys. Your input is vital in helping us map the current landscape and advance strategies that can save more young lives. Please see the links to the surveys below.
We encourage you to complete the survey specific to your specialty within the next two weeks. Your participation will directly contribute to shaping the future of pediatric transplant care. The results will be presented at the IPTA World Congress in 2025, where they will serve as a foundation for discussion, collaboration, and impactful change.
Please answer the survey that applies to your area of expertise.
Thank you for supporting this critical initiative and helping us build a brighter future for children who need transplants!
Your Opinions Matter!


December 2025 -
SMARTER Initiative





Become a Mentor Today!
Latest Tweets
Contact
Address
International Pediatric Transplant Association
c/o The Transplantation Society
740 Notre-Dame Ouest
Suite 1245
Montréal, QC, H3C 3X6
Canada