Newsletter 2016 Volume 13 - Issue 3

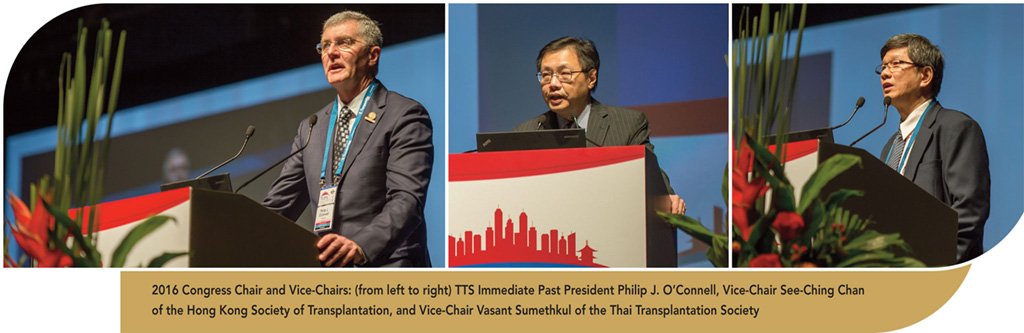
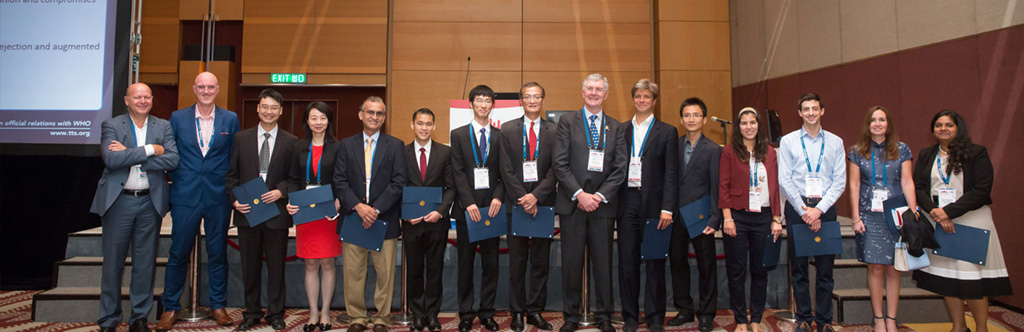
In August of 2016, the global transplant community gathered in Hong Kong, sharing advances in clinical medicine and experimental science at the 50th Anniversary Congress of The Transplantation Society
Over 3000 delegates from 85 countries met to exchange data, practice, and ideas
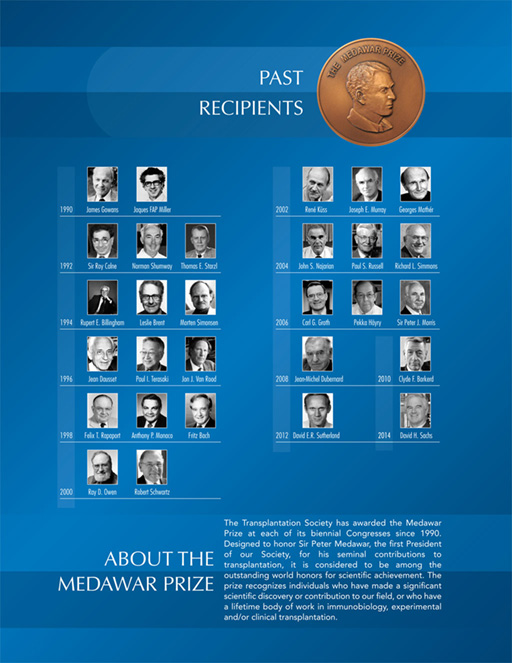
One of the highlights of the meeting was the award ceremony. Dr. Jan Lerut won the Award for Mentorship or Education and Training in Transplantation. Dr. Stan Jordan won the Outstanding Achievement in Clinical Transplantation Award (Clinical). Dr. Visist Dhitavat won the award for Outstanding Achievement in Transplantation (Developing Country). Dr. David Cooper won the award for Outstanding Achievement in Transplantation (Basic Science). Dr. S. Adib Hasan Rizvi won the Humanitarian Award in Transplantation. And Professor Jean Paul Soulillou won the prestigious Medawar Prize 2016 - the highest award of TTS.
21 Young Investigators were honored: Penelope Allen, Vaishnavi Calisa, Araving Cherukuri, Jason Davis, Denis Efimov, Shaimaa Elkholy, Jianing Fu, Barbara Kern, Qiang Liu, David N asralla, Kevin Tak-Pan Ng, Thomas Schachtner, Oscar Serrano, Rashmi Shingde, Umang Thakkar, Mirjam Tielen, Thomas Vanhove, Beorgios Vrakas, Johannes Wedel, Cheng Yang and Wai Ho Oscar Yeung.
24 mentor/mentee awards were bestowed by TTS in partnership with the Canadian Society of Trans-plantation, the Deutschen Trans-
plantationsgesellschaft, the Indian Society of Organ Transplantation, the Japan Society for Transplantation, the Nederlandse Transplantatie Vereniging, the Société-Française de Trans-plantation, the Sociedad Mexicana de Trasplantes, and the Transplantation Society of Australia and New Zealand.
Dr. Lori West received the Woman Leader in Transplantation Award and the WIT Hero Awards went to Dr. Elmi Muller and to Lalitha Raghuram.
Dr. Takemoto won the Leslie Brent Award for the most outstanding paper published in the field of Basic Science and Dr. Lucas won the Anthony P. Monaco Award for the most outstanding paper in the field of Translational Science Research.
The high level of intellectual exchange, outstanding venue and gracious hospitality of Hong Kong made for an enjoyable and productive meeting.
I look forward to meeting many of you over the coming two years at our Section meetings and the 2018 TTS Congress.
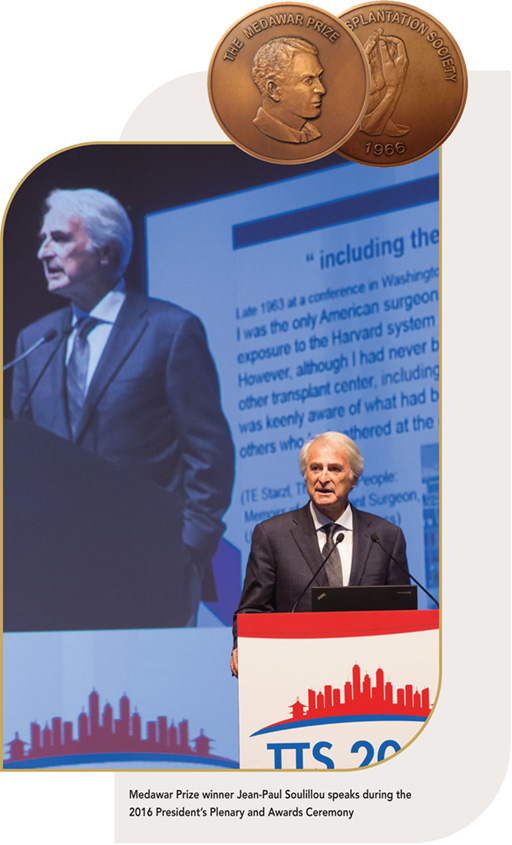
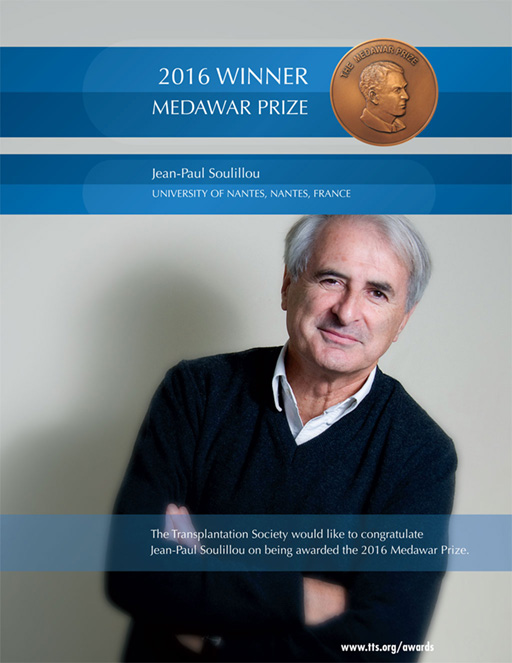
Jean-Paul Soulillou is Emeritus Professor of Immunology and has been the director of several INSERM Units. He was the founder of the Institute of Transplantation at Nantes University Hospital, one of Europe’s largest centers for research on transplantation sciences and clinical program for kidney and combined kidney-pancreas transplantations and of RTRS “Centaure”, a French translational network for transplantation sciences. He has been a member of the international advisory committee of the Immune Tolerance Network (ITN) of the NIH and past president of the Medical and Scientific Council of the French transplantation agency (Établissement Français des Greffes, EFG), and founder of the “Progreffe foundation” supporting research in science of transplantation.
Dr. Soulillou was also the first European to join the New England Journal of Medicine Editorial Board and served as Trustee of the International ROTRF Foundation. He was the founder and director of the RTRS “Centaure” and of the European Center for Transplantation Sciences and Immunotherapy. He holds the title of “Exceptional Class Professor” and was a senior member of the “Institut Universitaire de France.” He has been awarded several prizes including the Eloi Collery prize from the French Academy of Medicine, the Rayonnement Français prize, the 2008 International Award of the Transplant Society for his outstanding contribution to transplantation science (basic science) and the Prix d’Honneur 2012 of INSERM. He founded several biotech companies (Lynatec, Tc Land, Effimune and Xenothera).
Dr. Soulillou was one of the first to show the role of antibody in graft rejection. He introduced new treatments in humans (such as anti-IL2-R) and made important contributions in mechanisms of immune tolerance and rejection in kidney, heart and pancreas transplant and in multiple sclerosis. He is the author of more than 550 publications.

These awards recognize individuals who have made a major international impact in the field of transplantation. The awards are given out at each International Congress of The Transplantation Society.
David Cooper studied medicine at Guy’s Hospital Medical School of the University of London (now merged with King’s College London), where he also carried out research in heart storage for the PhD degree. He subsequently trained in general and cardiothoracic surgery in Cambridge and London before taking up an appointment in cardiac surgery at Groote Schuur Hospital in Cape Town. There, with Winston Wicomb, he developed a hypothermic perfusion device to store donor hearts, initially in large animals and subsequently in the clinical program. With Dimitri Novitzky, he investigated the detrimental effects of brain death on donor organ function in pigs and baboons before establishing thyroid hormone therapy in the management of potential organ donors in clinical transplantation. In 1987, he relocated to the Oklahoma Transplantation Institute in Oklahoma City where he continued to work in both the clinical and research fields; with colleagues, he identified the importance of the Gal antigen in xenotransplantation. After 17 years as a surgeon-scientist, he decided to concentrate his attention on research, initially in the TBRC at the MGH and subsequently at the Thomas E. Starzl Transplantation Institute at the University of Pittsburgh. For the past 25 years, his major interest has been the xenotransplantation of organs or islets in pig-to-nonhuman primate models.
After receiving his undergraduate and medical degrees from the University of North Carolina, Chapel Hill, Dr. Jordan completed a pediatric internship and residency at the University of California, Los Angeles. He completed three fellowships: one in pediatric nephrology at UCLA, one in experimental pathology in the Department of Immunology at Scripps Clinic and Research Foundation, and the third in dialysis and transplantation at Children's Hospital of Los Angeles. He is board certified in pediatrics, pediatric nephrology and diagnostic laboratory immunology.
For more than two decades, Dr. Jordan has performed extensive research into various aspects of immunology and transplantation, funded by dozens of research grants and awards, including two prestigious National Institutes of Health controlled clinical trials in kidney transplantation grants. He has written hundreds of articles and abstracts published in scientific journals, presented findings at medical and scientific organisations and authored about two dozen book chapters. Dr. Jordan's ground-breaking research in transplant immunology led to the development of a drug therapy protocol that significantly reduces the risk of a transplanted kidney being rejected.
Dr. Jordan has extensive experience with desensitization for incompatible kidney transplantation and currently has six investigator-initiated clinical trials examining novel therapies for desensitization and treatment of antibody-mediated rejection. He and his team pioneered the use of intravenous immunoglobulin to reduce the risk of rejection in difficult cases in which other medications failed. He also created a technique to detect post-transplant lymphoproliferative disorder in its earliest stages.

Dr. Visist Dhitavat has been the Director of the Thai Red Cross Organ Donation Centre since it was established in 1994. He is responsible for the development, maintenance and expansion of the whole process of organ donation and transplantation system in Thailand. He spends time and effort in giving knowledge and education, as well as in promoting positive attitudes toward organ donation both to the public and to healthcare professionals. He has been supported widely by all sectors: private, governmental and the media. Public awareness of organ donation has been raised through many means: news, educational materials and campaigns. He has developed good collaboration among healthcare professionals by visiting hospitals throughout the country to educate and persuade them to participate in organ donation process, and to push the organ donation to be a part of their routine work. In addition, he has set-up networks of in-house transplant coordinators at each hospital. Through these efforts, the rate of organ donation has increased by more than 10% per year.
For the last decade, Dr. Dhitavat collaborated on organ donation and transplantation meetings organized by the WHO. His aim is to achieve national self-sufficiency for organ donation and transplantation.

Jan Lerut, MD, PhD, trained in surgery at the Katholieke Universiteit Leuven (KUL), Belgium, under Prof. J. Gruwez; at the H. Heine University of Dusseldorf, Germany, under Prof. K. Kremer; and at the Université Catholique de Louvain (UCL), Belgium, under Prof. P.J. Kestens.
From the start of his surgical career, Dr. Lerut has been involved in organ transplantation. This interest resulted in a transplantation fellowship at the Universities Paris-Sud-Centre Hépatobiliaire Paul Brousse under Prof. H. Bismuth and at Pittsburgh Medical Centre under Prof. Thomas E. Starzl. He was Director of the Abdominal Transplant Program at the Inselspital University of Bern, Switzerland, from 1987 to 1991 (Prof. L.H. Blumgart).
Dr. Lerut is currently Professor of Surgery and co-Director of the Department of Abdominal and Transplantation Surgery, and Director of the Starzl Abdominal Transplant Unit at the University Hospital Saint Luc and the UCL Transplant Centre in Brussels.
Dr. Lerut has authored more than 300 peer-reviewed articles, 24 book chapters and 24 scientific films. He made more than 600 communications on national and international congresses, mostly devoted to liver transplantation. He co-edited the book Regenerative Medicine Applications in Organ Transplantation. His research interests focus on the development of technical refinements in liver transplantation, the value of liver transplantation in hepato-biliary oncology, the use of minimal immunosuppression and tolerance induction.

Professor S. Adibul Hasan Rizvi is the founder of Sindh Institute of Urology and Transplantation, Pakistan which started in 1971 and has progressed into the largest urology, nephrology and transplant centre of South Asia. It is based on the model of community government partnership. As a humanitarian, Prof. Rizvi’s mission has been to prove that everyone has the right to the best treatment that can be offered, and all of it free of cost.
Prof. Rizvi founded a high ethical standard transplant programme in Pakistan, the Sindh Institute of Urology and Transplantation (SIUT). SIUT has performed over 5000 living related kidney transplants with lifelong follow-up and immunosuppression free with dignity. He performed the first deceased kidney transplantation and initiated live related liver transplantation in the country with the help of Kings College and the Shiraz Organ Transplant Centre.
He has played a pivotal role in the campaign against transplant tourism and helped in the promulgation of transplant legislation to increase altruistic transplants and allow deceased donation. He is a Past President of the Middle East Society of Organ Transplantation; the Asian Society of Transplantation; the Nephrology, Urology, and Transplantation Society (NUTS) of the South Asian Association of Regional Cooperation (SAARC); and the Transplantation Society of Pakistan. He is a well known figure in the international scene and has been given several awards for his immense contributions in the field of medicine and transplantation, which include the Ramon Magsaysay Award, the St. Paul’s Medal, the Hunterian Professorship, the Felix T. Rapaport Award, the National Kidney Foundation Medal, and the Pioneer Award of the International Society of Nephrology (ISN).


Lori West, MD, DPhil, FRCPC, is an acknowledged leader internationally in the field of paediatric cardiac transplantation and immunology. Her pioneering clinical work in ABO incompatible infant heart transplantation has had an enormous impact in the field worldwide. This together with her laboratory investigations exploring the mechanisms of tolerance in the B cell compartment that develops in infants who receive an ABO incompatible graft has generated new insights in the field. Lori has taken leading roles at her own institution where she is Director of the Albert Transplant Institute and nationally where she pioneered the development of the Canadian National Transplant Research Programme, a multi-disciplinary research programme in transplantation across all of the provinces; Lori is currently Director of CNTRP.
Lori is an exemplary educator and mentor. She has trained, and continues to train, numerous highly qualified physicians and scientists, many of whom will be tomorrow’s academic leaders. Indeed, her trainees have won many awards from the major transplant professional societies and granting agencies.
Elmi Muller, MMed, MBChB, FCS, MRCS, FACS is the Head of the Transplant Unit at Groote Schuur Hospital in Capetown, South Africa, and directs an impressive clinical service at an institution with a rich history in transplantation. Through Elmi’s groundbreaking work in transplanting HIV positive organs from deceased donors into HIV positive recipients many South Africans are alive and off dialysis. Her work has had international impact on laws involving donation, including the introduction of the HIV Organ Policy Equity (HOPE) Act in the United States in 2014, ending the US federal ban on the procurement of organs from donors infected with HIV.
Elmi’s work with the transplant community goes well beyond her work with HIV positive donors, and includes volunteering her time with The Transplantation Society, the Women in Transplantation initiative, as an Executive Committee member of the Declaration of Istanbul Custodian Group (DICG) and her ongoing involvement in an international effort to bring renal transplant programs to the African continent.

Lalitha Raghuram’s role as a catalyst has brought together public and private hospitals, families, medical staff and public at large to take responsibility for organ donation. Her contribution in creating dedicated transplant coordinators, families, medical staff and public at large to take responsibility for organ donation. Her contribution is immeasurable, there are more than 1000 professionals have been trained so far with a direct impact of more than 5500 organs and tissues being transplanted to needy patients from deceased donors.
The transplant coordinator training is offered to all the interested and qualified individuals irrespective of their race, religion, gender, ethnicity, class, caste or creed. There are more than 500 women (more than 50%) that have been trained through this training program.
Lalitha Raghuram has been a mentor and an active board member of several hospitals has advocated for increasing women in transplantation be it doctors, nurses, or social workers. Her visionary untiring efforts along with MOHAN Foundation in India are on the path of saving many lives.

The recipients of the TTS Young Investigator Scientific Awards submitted abstracts to the Hong Kong transplantation Congress and received the highest scores from an international panel of reviewers.
Penelope Allen received a TTS Young Investigator Award for her research on Glomerulonephritis recurrence in kidney transplant recipients. Using data collected over 30 years (1985-2014) from the Australian and New Zealand Dialysis and Transplant Registry (ANZDATA), the study determined the incidence, risk factors, and outcomes of recurrent glomerulonephritis in kidney transplant recipients. The project was conducted under the supervision of Associate Professor Germaine Wong at the Centre for Kidney Research, Westmead in conjunction with the Sydney University School of Public Health.
Ms. Allen is currently studying postgraduate medicine at The Australian National University in Canberra, and will complete her MChD in 2018. She looks forward to being involved in ongoing research in the field of kidney transplantation. Penelope is a recipient of the Sydney University Summer Research Scholarship and the Transplant Society of Australia and New Zealand Young Investigator Award.
Vaishnavi Calisa received a Young Investigator Award for her work on the relative costs and health benefits of an age-matched deceased donor allocation algorithm compared to current practice, under the supervision of A/Prof Germaine Wong. A probabilistic Markov model was used to determine whether restricting the donor-recipient age-mismatch would improve graft and patient outcomes in different age groups. It was found that age-matching would provide small health benefits across the population, benefitting those between 30 and 60 but slightly disadvantaging those under 30 and over 60.
Ms. Calisa is currently in her second year of Bachelor of Science (Advanced) and Doctor of Medicine at The University of Sydney. Her current research interest is in using mathematical and statistical modelling in medical applications, particularly kidney transplantation. In April 2016 she received the Astellas Clinical Presentation Award and Young Investigator Award at the Transplant Society of Australia and New Zealand Annual Scientific Meeting.
Aravind Cherukuri received a Young Scientific Investigator Award for his work analysing de novo DSA and its relationship with the development of early T cell mediated rejection and chronic allograft histological changes. The study revealed that de novo DSA is associated with the development of early T cell rejection (TCR) and that the combination of DSA and TCR is associated with significantly worse renal function and chronic allograft injury than DSA alone. Further, in patients with DSA, a pro-inflammatory B lymphocyte cytokine profile predicted those at risk of TCR with a specificity of 100% and a sensitivity of 78%. Thus de novo DSA is a marker for a heightened cellular alloresponse and the study of B lymphocytes may potentially help to risk stratify patients allowing for early therapeutic intervention.
Dr. Cherukuri received his MBBS from Guntur Medical College and completed his residency and fellowship training in Nephrology at St. James’s University Hospital. He has an interest in transplant immunology and has taken up translational research in human kidney transplantation centred on cytokine expressing B lymphocytes. He received a PhD from the University of Leeds, and was a post-doctoral fellow at the Thomas E. Starzl Transplantation Institute. Dr. Cherukuri’s research is aimed at understanding the biology of cytokine expressing B cells in the context of immunological tolerance and developing predictive biomarkers for renal transplant rejection.
Jason Davis received a Young Investigator Award for his work on the Changes in Liver Allograft Steatosis and its Impact on Early Graft Function and Long Term Survival. Jason completed his work under the supervision of Dr. Richard S Mangus, the Surgical Director of Small Bowel and Multivisceral Transplantation at the Indiana University School of Medicine (IUSM). Results of the study confirm that there is a marked post-transplant decrease in liver steatosis. Overall, allografts with moderate to severe steatosis have worse early injury, delayed graft function, more substantial acute decrease in renal function, and worse survival. The subgroup analysis showed that transplant recipients who are younger, male, obese, or have fatty liver disease are more able to clear steatosis in the early post-transplant period compared to others.
Jason Davis is currently completing his M.D. from the Indiana University School of Medicine. He has completed multiple projects, receiving various awards and a fellowship in recognition for his work, most recently first place at the 2016 Association for Academic Surgery (AAS) Outstanding Medical Student Presentation. Also the 2015 Carolyn L. Kuckein Student Research Fellowship from the Alpha Omega Alpha (AOA) Honor Medical Society, which has helped him to expand on his other research endeavors in the transplant lab at the IUSM.

Denis Efimov was granted a Young Investigator Award for his research paper on DAMP-associated preservation injury and complications after liver transplantation. The results of the study showed that more severe DAMP-associated ischemia reperfusion liver graft injury was associated with higher incidence of severe early allograft dysfunction and lower incidence of acute rejection. Also it was revealed that donor polymorphism of TLR-4 gene in SNP rs913930 was associated with severe EAD occurrence after DBD LTx in Eastern European (Belarus) patients. This fact may help to stratify donors' grafts on high/low risk of EAD incidence based on genetically proved predictors.
Denis Efimov earned his MD on clinical medicine from Belorussian State Medical University in 2011. Currently, he works at the Republican Scientific and Practical Center for Organ and Tissue Transplantation (Minsk, Belarus). His research interests are: ishemia reperfusion injury, biomarkers, EAD prophylaxis after liver transplantation. He received the best presentation award at EFTW in 2014 (ESOT, Prague).
Shaimaa Elkholy received a Young Investigator Award at for her research on the predictors of mortality in living donor of liver transplantation (LDLT). This work represented a retrospective analysis for LDLT in Cairo University, which is the only source of donation in Egypt. This Unique experience was based only on living donation for which a risk index had been provided for prediction of early mortality. This risk index included MELD score, duration of ICU stay, and intra-operative blood transfusion with cut off values of 20, 9 and 8, respectively.
Dr. Elkholy graduated from Cairo University and she is now a lecturer at the Internal Medicine Department (Hepatogastroenterology Unit) Faculty of Medicine, Cairo University. She earned her phD in infections post liver transplantation, also from Cairo University. Her main interest is in Liver transplantation and GI endoscopy. She also received the Best Abstract award at the Pan Arab Liver Transplantation Society(PALTS) in 2013 for her research into nutrition in liver cirrhosis.
Jianing Fu was granted a Young Investigator Award for her research paper into naïve donor-derived lymphocytes from graft-resident lymphoid progenitors. Mixed lymphocyte reaction and high throughput TCRb CDR3 DNA sequencing were used to identify alloreactive T cell clones, and they were further tracked in blood or allograft post-transplant. The data demonstrated that donor graft-versus-host-reactive T cells and hematopoietic stem cells and progenitor cells carried within the graft play a key role in promoting and maintaining donor chimerism in the peripheral blood, which correlates with better clinical outcomes. This study provides new insights into the underlying mechanism of blood mixed chimerism and paves the way to develop new strategies to reduce graft rejection and achieve tolerance.
Dr. Fu received her MS on Chemical Biology from Peking University in China, and PhD on Cancer Biology and Immunology from University of South Florida. She is now a fellow at the Columbia Center for Translational Immunology at Columbia University. Under Dr. Megan Sykes’s mentorship, Dr. Fu’s research is aimed at decoding the bidirectional alloreactivity after intestinal transplantation and investigating the phenotype and function of gut hematopoietic stem cells and progenitors, with the ultimate goal of eliminating graft rejection by inducing long persistent blood mixed chimerism.

Dr. Barbara Kern received a TTS Young Investigator Award for her work on “Nonalcoholic steatohepatitis (NASH) as indication for Liver Transplantation in Europe - Clinical Analysis of over 37.000 patients”. This study investigates all adult patients with NASH, who underwent LT in Europe between 2002 and 2012 in collaboration with the ELTR registry in order to define risk factors and recommendation for this new epidemic.
Dr. Kern received her medical degree from the Medical University of Vienna. She is now a permanent resident at the Department of Visceral-, Transplant- and Thoracic Surgery at the Innsbruck Medical University, where she is also actively enrolled in the PhD program. To finish part of her thesis, she also spent one year abroad as a research fellow at the Johns Hopkins University, School of Medicine, in Baltimore, USA. Her research interests are in the field of liver, small bowel, and reconstructive transplantation.
Qiang Liu was granted a Young Investigator Award for his research on triglyceride exportation and lipid metabolism in the preservation of discarded steatotic human livers using 24 hours ex vivo normothermic machine perfusion. The study was the first to determine the lipid profile of the perfusate in ex vivo human liver normorthermic perfusion, and indicate that active triglyceride metabolism and exportation occur ex vivo regardless of transaminase release and bile production. It is the basis to reduce steatosis in human donor liver prior to transplantation by using prolonged perfusion and/or proper pharmacological intervention for eventually expanding donor criteria.
Dr. Liu earned his MD in China, mastering in medical imaging; and his PhD in biomedical science at the University of Leuven in Belgium. He also has a MSc in applied statistics. After working in Massachusetts General Hospital, Harvard University, he is currently doing research at the Cleveland Clinic with interest on ex vivo organ perfusion, assessment, and resuscitation prior to transplantation

David Nasralla was awarded a Young Investigator Scientific Award for his presentation of the results from a multinational randomised controlled trial comparing normothermic machine perfusion (NMP) with static cold storage (SCS) in human liver transplantation. This is one of several trials being conducted by the Consortium for Organ Preservation in Europe (COPE) and required 220 livers to be transplanted in 7 transplant centres in 4 EU countries. NMP was shown to substantially improve early graft function as measured by the peak-AST (primary outcome, p<0.01) and early allograft dysfunction rates (p<0.01) despite better organ utilisation and longer preservation times in the NMP group.
David graduated from the Oxford University Medical School in 2005 and is currently completing his surgical training in the Oxford Transplant Centre whilst writing up his DPhil under the supervision of Prof. Peter Friend. In parallel to this, he is collecting the longer-term follow-up data from the trial and remains actively involved with further NMP studies including planning the next phase of clinical trials. Other aspects of his research have been concerned with the uptake of bile salts during ex-vivo liver perfusion and using NMP to immunologically modify an organ.
Kevin Tak-Pan Ng was granted a Young Investigator Award for his research paper: Up-regulation of GSTA2 at early-phase after liver transplantation increases the risk of late-phase hepatocellular carcinoma recurrence. The study has demonstrated that up-regulation of hepatic and plasma GSTA2 at early-phase after liver transplantation indicates not only an increased early-phase hepatic injury and but also a higher risk of late-phase HCC recurrence after liver transplantation. GSTA2 played important roles in liver cancer cells to adapt the dynamic change of ROS condition during the course of liver transplantation. Targeting suppression of GSTA2 is possibly a novel strategy to reduce the likelihood of HCC recurrence after liver transplantation.
Dr. Ng received his PhD degree in the Department of Surgery, at the University of Hong Kong. Currently, he is working on identifying biomarkers and therapeutic targets that can predict and overcome liver cancer recurrence after liver transplantation. He is also a 2-time recipient of a Young Investigator Award from the International Liver Transplantation Society.
Thomas Schachtner was granted a Young Investigator Award for his research paper: Kinetics of CMV-specific T-cells from pre- to posttransplantation predict outcomes in CMV-seronegative kidney transplant recipients. His work suggests that monitoring CMV-specific T-cell kinetics from pre- to post-transplantation offers superior risk stratification of CMV-seronegative kidney transplant recipients from CMV-seropositive donors. He proposed that patients with stable/increasing CMV-specific T-cells are suspected to have protective immunity against CMV, and qualify for safe discontinuation of CMV prophylaxis. In contrast, patients with undetectable/decreasing CMV-specific T-cells are at increased risk of CMV-infection and should continue CMV prophylaxis and monitoring of CMV-specific cellular immunity.
Dr. Schachtner received his M.D. from the Charité University Medicine in Berlin, Germany. Currently, he is focused on the final year of his specialist training in nephrology and the completion of the habilitation procedure. His research interests are: characterization of virus-specific immunity in kidney transplant recipients with CMV- and BKV-infection, characterization of alloreactive cellular immunity in kidney transplant recipients, infectious complications after solid organ transplantation, and long-term outcomes of living kidney donors.
Dr. Oscar K. Serrano received a Young Investigator Award for his research project titled: Defining the Tipping Point in Surgical Performance for Laparoscopic Donor Nephrectomy Among Transplant Surgery Fellows: a Risk-Adjusted Cumulative Summation Learning Curve Analysis. Along with his colleagues at the University of Minnesota, Dr. Serrano performed a retrospective intraoperative case analysis to assess the learning curve of transplant surgery fellows performing laparoscopic donor nephrectomies (LDN). Based on their estimates, transplant surgery fellows require between 35 and 38 cases to become proficient with LDN but demonstrate a tipping point of learning the procedure by approximately 24 to 28 cases. This project is significant for setting standards for the training of transplant surgery trainees and defining a benchmark on the number of LDN operations needed to become proficient.
Dr. Serrano received his MD from Stanford University and his MBA from the Johns Hopkins University. He completed his General Surgery residency at the Albert Einstein College of Medicine and is now a fellow in Transplant Surgery at the University of Minnesota. Clinically, he is interested in all facets of abdominal organ transplantation and hepatobiliary surgery and his research interests integrate practice improvement with biomedical research innovation to improve patient care. He also takes great interest in the education and training of surgical trainees in the modern era.
Rashmi Shingde received a Young Investigator Scientific Award for her systematic review of unexpected donor-derived infectious transmissions in kidney transplants. Under the supervision of Associate Professor Germaine Wong at the Centre for Kidney Research, Westmead, Australia, her work showed that unexpected donor transmissions can have significant patient morbidity and mortality. Whilst rare, the true incidence of such events is unknown due to the lack of a standardised global reporting framework.
Ms. Shingde is currently studying Medicine at the University of New South Wales and has an interest in renal and endocrine medical research.
Umang G. Thakkar was granted a Young Investigator Award for his research paper on Stem cell therapy for post-traumatic paraplegia and for renal parenchymal diseases. Autologous/ allogeneic mesenchymal stem cells (MSCs) can be generated in vitro from adipose tissue. MSCs have no HLA markers, are tolerogenic and immunomodulatory. Hence they can be used in immune disorders/ transplantation/ regenerative medicine. Neuronal differentiated autologous adipose tissue derived mesenchymal stem cells (Ad-MSCs) along with hematopoietic stem cells (HSCs) infused into cerebrospinal fluid for post traumatic paraplegia. Allogenic Ad-MSCs and HSCs were infused into portal, thymic and renal circulation for remission of renal parenchymal diseases. Post traumatic paraplegia which has no hope of recovery, can be treated with neuronal differentiated autologous Ad-MSCs and HSCs. Progression of RPD to ESRD can be arrested/ halted by Ad-MSCs and HSCs.
Mr. Thakkar earned his DCH (Paediatrics) from India and is experienced in the field of regenerative medicine. Currently he is working at the G.R. Doshi and K.M. Mehta Institute of Kidney Diseases & Research Centre (IKDRC) - Dr. H.L. Trivedi Institute of Transplantation Sciences (ITS), Ahmedabad, India. His research interests are stem cell therapy for treatment of various neurological disorders, cardiac disorders, autoimmune diseases like type-1 diabetes mellitus, systemic lupus erythematous etc.
Mirjam Tielen received a Young Investigator Award for her work on medication adherence after kidney transplantation. In collaboration with Emma Massey, Assistant Professor Health Psychologyof the Erasmus Medical Centre of Rotterdam, she has performed several studies on adherence of kidney transplant patients. In this particular study it was found that patients who reported being non-adherent to immunosupressive medication had a lower 4-year graft survival compared to adherent patients.
Ms. Tielen is a nurse practitioner with more than 10 years’ experience in the field of adult kidney transplantation at the Erasmus University Medical Center in Rotterdam. In her work as a nurse practitioner she works mainly at the outpatient clinic, evaluating transplant candidates and their living donors as well as providing post-transplant care. She obtained a PhD degree on 6th April 2016. She is an active member of several nursing organizations and was, for example, the President of the Dutch Workgroup of Transplant Nurses for 5 years. Currently, she is a board member of the Nurse Practitioner Society in the Erasmus Medical Center of Rotterdam and has also been board member of the foundation of OWVS (supporting scientific research among nurse practitioners) since 2013. In the future she will continue her work on medication adherence after kidney transplantation and she will focus on interventions to promote adherence to improve clinical outcomes.
Thomas Vanhove received a Young Investigator Award for his research related to connective tissue growth factor (CTGF). CTGF expression in 3-month renal allograft protocol biopsies was predictive of the progression of interstitial fibrosis on repeat 5-year biopsies, together with donor age. This indicates that, in a cohort of low-risk renal recipients with favorable histology at 3 months, significant differences may exist in the activation of profibrotic pathways, with implications for the development of long-term fibrosis. These findings are largely in agreement with previous microarray data that suggest important profibrotic and inflammatory activity, even in allografts with benign histology.
Thomas Vanhove received his MD from the Catholic University of Leuven, Belgium. He completed a residency in Internal Medicine at the University Hospitals Leuven and currently works as a research fellow at the Department of Nephrology and Renal Transplantation. His research focuses on tacrolimus pharmacology and identifying predictors of long-term renal allograft histology.
Georgios Vrakas received a Young Investigator Award for his work on the immunological impact of simultaneous intestinal and vascularized composite allograft transplantation at the Oxford Transplant Centre. The development of de novo donor specific antibodies (DSAs) after an intestinal transplant, in line with other organ types, is detrimental to the long-term outcome of the graft. So far, the Oxford data suggests that combining an abdominal wall vascularised composite allograft with an intestinal transplant does not increase the incidence of de novo DSAs. Dr. Vrakas received his MD from the
University of Crete, Heraklion, Greece, his M.Sc. from the Dimokrition University, Alexandroupolis, Greece and his Ph.D. from the Aristotle University, Thessaloniki, Greece. He was a resident for General Surgery at Drama and Papanikolaou General Hospitals, Greece. After his board certification as a Specialist for General Surgery, he completed transplant fellowships at Guy’s Hospital, London, UK and Churchill Hospital, Oxford, UK. Currently he is a Consultant Transplant Surgeon at Oxford University Hospitals. Clinically he is interested in intestinal and multivisceral transplantation and in renal autotransplantation following ex vivo resection of conventionally unresectable renal neoplasias. His research interests are: determining sentinel markers tracing status of the transplanted organ and remote, patient led, monitoring.

Johannes Wedel received a Young Investigator Award for his work on the identification of DEPTOR as a novel regulatory molecule in the alloactivation of CD4+ T cells. DEPTOR is a first-in-kind cell intrinsic modulator of mTOR, which Dr. Wedel demonstrated is expressed in T cell subsets and serves to enhance immunoregulation in vitro in cell culture models and in vivo in a fully MHC mismatched model of cardiac allograft rejection. The survival of wild type grafts in DEPTOR transgenic (overexpressors) is significantly prolonged (p<0.05). His studies provide for the intriguing possibility that targeting the regulation of DEPTOR in T cells has promise as a future therapeutic.
Dr. Wedel received his MD from Heidelberg University, Germany, and his PhD from the University of Groningen, The Netherlands. He is currently training as a research fellow in the Briscoe Laboratory and the Transplant Research Program at Boston Children’s Hospital, USA. He is interested further developing his career as a physician scientist in transplantation, and wishes to develop a research effort focused on alloimmunity and the identification of intracellular signals pathways pertinent to T regulatory cell survival and function post-transplantation.
Dr. Cheng Yang received a Young Investigator Award for his work on the cyclic helix B peptide inhibition ischemia reperfusion-induced renal fibrosis via the PI3K/Akt/FoxO3a pathway. In collaboration with Prof. Yaqiu Long in SIMM, Chinese Academy of Sciences, they recently synthesized a novel proteolysis-resistant cyclic helix B peptide (CHBP) that exhibits promising renoprotective effects. In this study, Dr. Yang evaluated the effect of CHBP on renal fibrosis in an in vivo ischemia reperfusion injury (IRI) model and in vitro TGF-β-stimulated tubular epithelial cells (TCMK-1 and HK-2) model. Their findings demonstrate that CHBP attenuates renal fibrosis and the epithelial-mesenchymal transition of tubular cells, through suppression of the PI3K/Akt pathway and thereby the inhibition FoxO3a activity. CHBP may become a promising new drug for the treatment of renal fibrosis.
Dr. Yang received his MD and PhD from the Fudan University in Shanghai. He then completed his surgical residency at Zhongshan Hospital, Fudan University. During the PhD training, he visited University Leicester and collaborated with Prof. Bin Yang on the research of acute kidney injury. He is now a resident in the Department of Urology at Zhongshan Hospital. In addition to TTS, Dr. Yang is a member of AST and ESOT. His research interests include acute kidney injury, rejection and tolerance, immune regulation in transplantation and cell apoptosis/necroptosis.

Oscar Yeung received a Young Investigator Award for his work with the topic "Transforming growth factor beta receptor III (TGFβR3) induced tumor promoting macrophages via complement component C5a in liver cancer". Following his previous study on the identification of M2 macrophages as one of the critical mediators in hepatocellular carcinoma (HCC) development, Dr. Yeung shifted his research focus to the mechanisms of tumor cells used for recruiting and stimulating the macrophage populations in the tumor microenvironment. In the study, he showed that that loss of the TGFβR3 contributed to the increased M2 macrophages in HCC through activating the complement component systems.
Dr. Yeung received his PhD from the University of Hong Kong and currently a post-doctoral fellow in the Department of Surgery. His research projects focus on the innate immunology particularly macrophages in liver transplantation and HCC.

The Transplantation Society (TTS) along with the collaboration of its Affiliated Societies celebrates the contributions of basic science to the field of transplantation by recognizing the efforts of basic scientists who have advanced our understanding of transplant science/immunobiology and/or treatment of transplant recipients, and the young investigators who will be the future leaders in transplantation.
This award was made possible with the joint contribution of the Canadian Society of Transplantation (CST) and TTS.


Prospective Treatment and Novel Biomarkers of BK Polyomavirus Associated Nephropathy
Minal Borkar received Mentee-Mentor Award for her work “Prospective treatment and novel biomarkers of BK polyomavirus associated nephropathy”. This project gave significant piece of information about the mechanisms by which BK polyoma virus causes these changes eventually leading to graft loss and patient morbidity. It will also help in the identification of novel biomarkers of cell death and Epithelial Mesenchymal Transition which will eventually lead to better diagnosis and prognosis of BK nephropathy. The more research on understanding the mechanism will help in establishing clinically proven effective antiviral treatment for BK PVAN.
Minal Borkar is a postdoctoral research fellow with Dr. Lee Anne Tibbles at University of Calgary since November 2012. She has received Canadian National Transplant Research Program (CNTRP) fellowship in 2014 and cleared another CNTRP- Alberta Transplant Institute Fellowship in 2015. Minal worked as a Postdoctoral Fellow in Spain and Scientist in Department of Medical Genetics at Sir Ganga Ram Hospital, India. She is the recipient of various awards like Mentee-Mentor Award BSM 2013 Paris, AST-IDCOP Travel Award in American Transplant Congress 2016, CNTRP Travel Award for World Transplant Congress 2014 and twice Nick Norgan award for the best paper of the Journal in 2010 and 2012
These awards were made possible with the joint contribution of the Deutsche Transplantationsgesellschaft (DTG) and TTS.

Metabolites Associated with Bariatric Surgery Reverse Accelerated Rejection and Augmented Alloimmunity in Obese Allograft Recipients
Dr. Markus Quante received the International Transplantation Science Mentee-Mentor Travel Award in for his work on the impact of obesity on alloimmune responses in a mouse transplant model. He showed that obesity accelerated allograft rejection linked to a more pronounced pro-inflammatory immune response. Weight loss subsequent to bariatric surgery, in contrast, prolonged allograft survival and skewed the immune response towards Th2 dominated conditions. Metabolic changes that were linked to bariatric surgery modified alloimmune responses and prolonged graft survival. These results will serve as a basis for a future detailed mechanistic analysis.
Dr. Quante received his MD from the Hannover Medical School, Germany, completed his surgical residency at the University Hospital Leipzig, and afterwards a member of the IFB Integrated Research and Treatment Centre Adiposity Diseases. In July 2013, Dr. Quante joined the Transplant Surgery Research Laboratory at Brigham and Women´s Hospital in Boston as a postdoctoral research fellow. Dr. Quante is currently at the Department of General-, Visceral-, and Transplantation Surgery in Tuebingen, Germany.

Cell-free Mitochondrial DNA Activates DCs in an Age-dependent Fashion and Compromises the Survival of Older Grafts
In 2016 Sebastian Stead was awarded the International Transplantation Science Mentee-Mentor Travel Award in recognition for his abstract entitled: Dendritic cell phenotype and function modification with targeted porous silicon nanoparticles. His work is focused on identifying novel treatments within the field of nanomedicine, providing alternative methods for delivering immunosuppressive medications in an acute, localised fashion. Functionalisation of the nanoparticles has shown the ability to provide enriched delivery to myeloid dendritic cells, one of the least abundant cells within the body. The composition of the nanoparticles allows them to be tailored for specific therapy, capable of being loaded with a myriad of drugs or coated with different antibodies, permitting cell specific targeting.
Sebastian is currently a PhD candidate in Medicine, at the University of Adelaide in Australia, under the supervision of Professor P. Toby Coates. His research is focused on utilising nanoparticles to induce antigen specific tolerance within type 1 diabetics, and if successful, it may have the potential to improve the lives of millions of sufferers. The clinical applications could also be tailored to help deliver drugs to treat cancers more specifically than current chemotherapeutic methods, or have positive ramifications in the manufacture of more effective vaccines.
These awards were made possible with the joint contribution of the Indian Society of Organ Transplantation (ISOT) and TTS.


Peripheral NK-cell Repertoire Distribution in Chronic Allograft Dysfunction after Renal Transplantation
Sailaja Kesiraju completed her Post-doctoral fellowship at Bhagwan Mahavir Medical Research Centre, Hyderabad. Her current on-going five year research project has the rubric “Non Invasive Diagnosis of Acute Rejection and Methods to Monitor Graft Survival in Renal Transplant Patients”; the work is being carried out in the Immunology department at the Bhagwan Mahavir Medical Research Centre. Dr.Sailaja received her Doctor of Philosophy award from Osmania University and her thesis was on the topic “Oxidant-Antioxidant Status of Serum and Roncho-alveolar Lavage in Common Respiratory Disorders”.
Dr. Kesiraju’s primary research goal is to find a non-invasive, accurate, sensitive and rapid diagnostic test for the early detection of rejection, chronic allograft dysfunction as well as tolerance of the allograft. A sensitive non-invasive test that is able to detect acute and chronic injuries in the transplant will be a very useful adjunct in clinical practice to monitor the graft function.

Impact of Single Centre Kidney Paired Donation Transplantation to Increase Donor Pool in India
Vivek Kute received the International Transplantation Science Mentee-Mentor Award 2016 recognizing his work on “Impact of Single Center Kidney Paired Donation Transplantation to Increase Donor Pool in India” under mentorship of Prof HL Trivedi and Prof PR Shah.
Vivek Kute is Associate Professor of Nephrology and Transplantation at Institute of Kidney Diseases and Research Center and Dr. HL Trivedi Institute of Transplantation Sciences, (IKDRC-ITS) and the Gujarat University of Transplantation Sciences (GUTS) Ahmedabad, India. He has received various awards for his major contributions in the field of transplantation, including a Young Investigator award 2012 in Berlin, Bansal Oration and Janseen-Cilag award by Indian Society of Nephrology, and Udupa Memorial Lecture 2015 by ISOT. He is a mentor for the Young Nephrologist Mentoring Program for ISN. He has published over 100 research papers in peer reviewed journals and made oral presentations in various national and international conferences. His research involves expanding donor pool with kidney-paired donation transplantation.
Development of De-novo Donor Specific Antibody (DSA) and Vitamin D Status after Renal Transplantation

Ultra-high Resolution Non-contrast Imaging for Chronic Rejection Monitoring and Procedural Planning in Reconstructive Transplantation
Shailesh B. Raval received a Mentor-Mentee Award for the developmental work on the non-invasive, non-radiation, contrast-free, ultra-high resolution (UHR), 3D nerve and vascular MRI imaging method in conjunction with RF imaging system. Our approach is renal-toxic-contrast and radiation-free, increasing its safety in Reconstructive transplantation (Craniofacial or Upper Extremity) or even Solid Organ transplantation (especially renal transplant) applications for sequential non-invasive graft monitoring of Chronic Rejection (CR). These could include intimal, luminal and flow parameters reflective of CR related vascular changes that may result in ischemic graft attrition or loss in RT or in SOT. In addition, Nervetractography can monitor neuroregeneration after transection, repair or transplant related nerve outcomes.
Shailesh is completing his PhD in Bioengineering (in collaboration with Radiology and Plastic Surgery) from the University of Pittsburgh. His current work includes development of unique RF imaging systems and exploring cutting edge medical imaging applications in various body organs.

Imbalance of T Helper 17 Cells and T Regulatory Cells is Associated with Chronic Active Antibody Mediated Rejection in Renal Allograft Recipients
Brijesh Yadav is a final year PhD student under Prof. Narayan Prasad in the Department of Nephrology and Renal Transplantation at Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, India. His PhD thesis is on “Regulatory, effector and cytotoxic T cell profiles in chronic renal allograft dysfunction”, profiling regulatory, effectors and cytotoxic T cell subsets frequency by Flowcytometry, Serum and PBMC culture supernatant cytokines by ELISA, intragraft infiltrations of above T cell subsets by quantitative real time PCR and Immunohistochemistry in biopsy proven renal allograft recipient patients of chronic active antibody mediated rejection, calcineurin inhibitor toxicity and idiopathic transplant glomerulopathy. He has been awarded with Newton-Bhabha Fellowship for research training at Cambridge University by the British Council, Best Abstract award by the Asian Society of Transplantation Singapore (CAST-2015), Young Scientist awards by Invertis University India, Abstract of Distinction award by Gujarat University of Transplantation Science, and the DST-INSPIRE Senior Research Fellowship by DST, Govt. of India.
These awards were made possible with the joint contribution of the Japan Society for Transplantation (JST) and TTS.

Systemic Therapy of Regulatory Dendritic Cells Derived Form Induced Pluripotent Stem Cells allows Allogeneic Cardiac Grafts Acceptance
Songjie Cai received a Mentee-Mentor Award for her work with systemic therapy of regulatory dendritic cells. In collaboration with Dr. Xiao-Kang Li’s lab at National Research Institute for Child Health and Development (Tokyo), dendritic cells (DCs) were generated and characterized from murine induced pluripotent stem cells (iPSCs). Dr. Cai identified that donor-type iPSCs derived DCregs (iPS-DCregs) could lead to permanent acceptance of fully MHC-mismatched murine allogeneic cardiac grafts, but rejected third-party allografts. She also found that preconditioning of donor-type iPS-DCregs to recipients generated antigen-specific regulatory T cells (Tregs), which is in association with TGFβ.
Dr. Cai got her MD in clinical medicine from Shanghai Jiaotong University (China), completed her Surgery residency at Shanghai East Hospital, and her PhD on medicine science from Osaka University (Japan). Her research interests are immunobiology of dendritic cells during immune response to transplantation alloantigen. Under Dr. Shiro Takahara’s mentorship, Dr. Cai’s research focused on understanding the basic processes that control dendritic cells maturation, activation and migration with the ultimate goal of enabling clinicians to cell therapy and immunosuppression monitoring.
Various Pathogenic Microbes Induce CNI-resistance in B-cells Responding to Blood Group Antigens through TLR–MyD88 Pathway
Hiroshi Sakai received a Mentor-Mentee award for his work with pathogenic microbes. He focused on the influence of toll-like receptor signaling, through the binding of bacterial-derived ligands, on B cell activation in response to blood group carbohydrate-antigens, because bacterial infection following ABO-incompatible organ transplantation has been reported to be associated with refractory antibody-mediated rejection. This study provides the first evidence that B-cells responding to blood type A carbohydrate, in the presence of toll-like receptor-MyD88 signaling, show the sIgM+CD5dim/-B-1b phenotype, and lose susceptibility to inhibition by CsA, following ABO-incompatible transplantation.
Dr. Sakai received his MD from Hirosaki University, and is now a PhD student in Gastroenterological and Transplant Surgery at Hiroshima University. Under Dr. Hideki Ohdan and Dr. Yuka Tanaka’s mentorship, Dr. Sakai’s research is aimed at regulating B cells responding to carbohydrate antigens in allo- and xeno-transplantation.

Clinical and Immunological Significance of Controlling Portal Vein Pressure in Living Donor Liver Transplantation
This award was made possible with the joint contribution of the Nederlandse Transplantatie Vereniging (NTV) and TTS.

Belatacept Fails to Inhibit Donor-reactive Tfh-B Cell Interaction but Favors a Regulatory Transitional B Cell Profile Over Tacrolimus
Gretchen de Graav received a Mentee-Mentor award for her research on the effects of belatacept on follicular T helper-B cell interaction in kidney transplantation. Under supervision of Dr. Carla Baan at the Transplantation Laboratory at Erasmus University Rotterdam, the donor-antigen driven formation of plasmablasts was compared between cultures spiked with belatacept and tacrolimus. Cells were obtained from 40 kidney transplant patients randomized to a belatacept-based or tacrolimus-based immunosuppressive regimen. Unlike in animal studies, plasmablast formation was not inhibited by belatacept, but only by tacrolimus. The survival of regulatory IL10+ transitional B cells was, however, favored in the presence of belatacept, but diminished by tacrolimus. The question remains which patients can benefit from and which patients are burdened with the attenuated inhibitory effects of belatacept on Tfh-B cell interaction.
Dr. de Graav received her MD from the Erasmus Medical Center University. Currently, she is finishing her PhD project and she will start her Internal Medicine Residency at the Maasstad Hospital, Rotterdam.
This award was made possible with the joint contribution of the Société Française de Transplantation (SFT) and TTS.
Interleukin-34 is a Treg-specific Cytokine and Mediates Transplant Tolerance
Dr. Séverine Bézie received a Mentee-Mentor Award for her work on Interleukin-34, a Treg-specific ucytokine that mediates transplant tolerance, Under the mentorship of Dr. carole Guillonneau. In a translational study from rat to human, she showed that IL-34 has immunoregulatory properties, inducing tolerance to the allograft and delaying GVHD. Moreover, it was shown that this cytokine is specifically expressed by Foxp3+Tregs and involved in their suppressive function, but also modulated macrophages polarization to expand Tregs in a feedback loop. These properties make it a promising candidate as tolerance inducer treatment.
Dr Bézie got her PhD from the Université de Nantes, France, focused on the identification of new immunoregulatory molecules in a rat model of transplantation. She currently works at the INSERM 1064 Center of Research in Transplantation and Immunology in Nantes, with interests in new therapies promoting allo-specific Tregs.
This award was made possible with the joint contribution of the Sociedad Mexicana de Trasplantes (SMT) and TTS.

Pre-transplant AT1Rabs are Associated with Acute Rejection in 2-Haplotypes Kidney Transplant Recipients
These awards were made possible with the joint contribution of the Transplantation Society of Australia and New Zealand (TSANZ) and TTS.


Surface Modification of Porcine Aortic Endothelial Cells with Corline Heparin Conjugate (CHC) Protects Against Xenogeneic Thrombosis and Inflammation
Anjan K. Bongoni received a Mentee-Mentor Award for his work on the surface modification of porcine aortic endothelial cells. In this study, the feasibility of using CHC to protect pig vascular endothelial cells against xenogenic coagulation and inflammation was tested in an in vitro pig-to-human xenotransplantation setting using a whole blood coagulation assay that closely mimics the in vivo small vessel endothelial surface-to-blood volume ratio. Results demonstrated that surface immobilization of the multi-arm heparin conjugate CHC has the potential to prevent the establishment of pro-coagulant and pro-inflammatory environment induced by xenotransplantation and thus may support the survival and function of porcine xenografts. Therefore, this strategy provides a possible therapeutic option to attenuate thromboinflammation in xenotransplantation.
Dr. Anjan Bongoni received his PhD in immunology from the University of Bern, mainly focused on the functional evaluation of multi-transgenes in genetically modified pigs for xenotransplantation. Currently, he is working as a post-doc fellow in the Immunology Research Centre (IRC) at St. Vincent’s Hospital Melbourne. His research interests are: identifying and testing novel reagents and regulators of the intravascular innate immune system (complement, coagulation and inflammation) in mouse models of renal ischemia-reperfusion injury and heart allotransplantation. He received Young Investigator Awards in the past from the International Xenotransplantation Association and The Transplantation Society.

Disruption of CD8-coreceptor Cinding Abrogates Tolerance Induction via Liver-directed Expression of Donor MHC Class I

Dendritic Cell Phenotype and Function Modification with Targeted Porous Silicon Nanoparticles
In 2016 Sebastian Stead was awarded a Mentee-Mentor Award in recognition for his work with dendritic cell phenotype and function modification. His work is focused on identifying novel treatments within the field of nanomedicine, providing alternative methods for delivering immunosuppressive medications in an acute, localised fashion. Functionalisation of the nanoparticles has shown the ability to provide enriched delivery to myeloid dendritic cells, one of the least abundant cells within the body. The composition of the nanoparticles allows them to be tailored for specific therapy.
Sebastian is currently a PhD candidate in Medicine at the University of Adelaide, under the supervision of Professor P. Toby Coates. His research is focused on utilising nanoparticles to induce antigen specific tolerance within type 1 diabetics.

Risky Organs: Trends in Comorbidities among Potential and Actual Australian Organ Donors in New South Wales 2010-2015
Imogen Thomson received a TTS/TSANZ Mentee-Mentor Award in conjunction with her supervisor, Associate Professor Angela Webster, for her abstract 'Risky Organs: Trends in Comorbidities among Potential and Actual Australian Organ Donors in New South Wales 2010-2015’. Ms Thomson’s research centred on characterising disease burden among organ donor referrals, and the impact that this has on the likelihood of a potential donor proceeding to donate.
Ms Thomson is currently in her second year of the Doctor of Medicine Program at the University of Sydney, and completed her undergraduate studies in Biomedical Science at Bond University, Australia. Under the mentorship of Associate Professor Webster, she is also undertaking a Master of Philosophy (Medicine) alongside her medical studies, with a focus on identifying opportunities to increase organ donation rates in New South Wales. She hopes to pursue a career in the field of transplantation in the future.
These awards were made possible with the contribution of The Transplantation Society (TTS).
Effect of Epigenetic Modifications in Graft Kidneys Progressing to Chronic Allograft Dysfunction
Dr. Sai Vineela Bontha received a Mentee-Mentor award for her work with epigenetic modifications in grafts. Mentored by Dr. Valeria Mas, this work evaluates the differences in DNA methylation patterns between renal allografts with histologic evidence of interstitial fibrosis and tubular atrophy which progress to chronic allograft dysfunction and those with normal histology and function. Differential DNA methylation patterns were studied in association with changes in gene expression patterns downstream using an integrative approach. Future studies are planned to identify the timeline associated with the changes in DNA methylation patterns and to delineate a cause-effect relationship between DNA methylation and allograft dysfunction.
Dr. Bontha received her PhD from Leibniz Graduate School on Aging and Jena University Hospital in Germany. She is currently a post-doctoral research associate at the Translational Genomics Transplant Laboratory at the University of Virginia. Her research interests include the identification of noninvasive biomarkers that predict short- and long-term graft outcomes, as well as furthering understanding of the underlying mechanisms leading to chronic renal allograft dysfunction.

Human Anti Thrombotic Genes do not Obviate the Need for Anticoagulation in Aiding Long-term Xenograft Survival
Joshua Chan was awarded a Mentee-Mentor Award for his work on the use of multi-transgene expression for prevention of cardiac xenotransplantation-associated consumptive coagulopathy. The novel use of six-gene modified cardiac xenografts, particularly the inclusion of humanized factors TFPI, DAF, and EPCR, was found to be associated with improved levels of multiple factors in the coagulation-fibrinolysis cascade. Prevention of post-xenotransplant critical consumptive coagulopathy may have significant implications for the potential clinical application of cardiac xenotransplantation.
Dr. Chan is a research fellow in the Cardiothoracic Surgery Research Program at the National Heart, Lung and Blood Institute (NHLBI), National Institutes of Health (NIH). His primary interest is in cardiac xenotransplantation, specifically in xenoimmunology, transgenic engineering, and transplant rejection. He received his Bachelors of Arts degree in Biology at New York University (NYU) and subsequently earned his medical degree from the University of Southern California Keck School of Medicine (USC). He went on to complete his internship at Cedars-Sinai Medical Center where he matriculated from his 3rd year general surgery resident prior to his current research sabbatical.
Vascular Sequestration of Donor-specific Antibodies Protects Allogeneic Islets from Humoral Rejection
Chien-Chia Chen was granted a Mentee-Mentor Award for a translational research project in which he combined the analysis of clinical samples with the use of murine models to explore the mechanisms of resistance of allogenic islets to antibody-mediated rejection. His work led to the conclusion that endothelial chimerism combined with vascular sequestration of alloantibodies explains why the rate of attrition of islet graft was not accelerated in the presence of alloantibodies. These results suggests that the alloantibodies should be seen as 'marker' of rejection rather then 'maker' in islet great recipients.
Dr. Chen received his MD and completed his surgical residency at the National Taiwan University. He is currently a PhD student under the supervision of Prof. Thaunat in INSERM U1111, Lyon, France. His researches focus mainly on deciphering pathophysiology of antibody-mediated rejection.

CD45RA Identifies TSDR Demethylated Regulatory T Cells with a Stable Phenotype and Suppressive Cytokine Profile
Rebeca Arroyo-Hornero was granted a Mentee-Mentor Award for her research paper “CD45RA Identifies TSDR Demethylated Regulatory T Cells with a Stable Phenotype and Suppressive Cytokine Profile”. Regulatory T cells are currently being tested as a cellular therapy in transplant patients aiming at promoting transplant tolerance and reducing levels of immunosuppression chemotherapy. Stable bona fide regulatory T cells can be accurately identified by the demethylated status of a specific DNA region called TSDR. However, for cellular therapy is crucial to identify cell surface markers sufficient to isolate cells that remain stable and potent after expansion and in the presence of immunosuppressive drugs. In comparison with CD45RA- regulatory T cells, CD45RA+ regulatory T cells retained more stable suppressive properties after in vitro expansion, also in the presence of low levels of calcineurin inhibitors. All suggests that CD45RA+ regulatory T cell population is a promising candidate for cell therapy and should be studied further.
Ms. Arroyo-Hornero received her Bachelor Degree in Biotechnology from the University of Murcia in Spain. Currently, she is a PhD student at the University of Oxford, studying cellular therapies for transplantation. She is interested in discerning how regulatory T cells suppress the immune response and the possibility of genetically modified regulatory T cells to potentiate and stabilize their suppressive activity.

AMP-activated Protein Kinase Attenuated Marginal Liver Graft Injury via Promoting Mitochondrial Biogenesis and Respiratory Function
Liu Jiang received a Mentee-Mentor Award for his work on the AMP-activated protein kinase attenuates marginal liver graft injury via promoting mitochondrial biogenesis and respiratory function. The specific gene favoring improving marginal graft survival was studied using hundreds of clinical liver transplant samples, rat model with small-for-size orthotopic liver transplantation and AMPK transgenic mice received I/R injury plus major hepatectomy. The key findings provide a possible way to ameliorate fatty graft injury by increasing activity of the kinase. Further study applying activators for activating this kinase is needed for clinical application.
Dr. Liu received his bachelor and master degrees in clinical medicine from Medical School of Nankai University in China. He is a current PhD student in the University of Hong Kong. His research interests are: mitochondrial function and marginal graft injury after liver transplantation, metabolism alternation during fatty graft injury, and surgical treatment for late phase liver diseases. He received a Young Investigator Award in the past from the International Liver Transplantation Society.
The Clinical Significance and Potential Therapeutic Role of GPx3 in Tumor Recurrence after Liver Transplantation
Qi Xiang received Mentee/Mentor Award as mentee for his research paper “The Clinical Significance and Potential Therapeutic Role of GPx3 in Tumor Recurrence after Liver Transplantation”. Under the instruction of Prof. Man, the research team identified that the down-regulation of GPx3 in small-for-size liver graft was significantly associated with HCC invasiveness in a rat model and lower plasma GPx3 was an independent predictor for poor overall survival of HCC patients after liver transplantation. Moreover, they found that GPx3 was not only a predictor for prognosis, but also suppressed HCC invasiveness through JNK-cJun-MMP2 signalling pathway. Therefore, in addition to prognostic value, GPx3 may possess the therapeutic potential targeting at HCC recurrence after liver transplantation.
Dr. Qi earned his MD in clinical medicine from mainland China and PhD on surgery from The University of Hong Kong. Currently, he works as post-doctoral fellow in Department of Surgery, The University of Hong Kong. His research interests are: explore the role of functional biomarker for tumor recurrence after liver transplantation. He received Mentee-Mentor Awards twice in the past from The Transplantation Society and is a 2-time recipient of a Young Investigator Award from The Liver Transplantation Society.

The Transplantation Science Committee of The Transplantation Society and Transplantation are pleased to announce the best manuscripts submitted to the Journal in 2016. Named after two pioneering giants, a selection committee that included editors of Transplantation, The Transplantation Society, in addition to members and chairs of the Transplantation Science Committee selected two winners amongst a very competitive group of applicants. An extended article on these awards will be published in the January 2017 edition of Transplantation.

Naohiro Takemoto, et al
The Leslie Brent Award for the Best Publication in Basic Transplantation Research went to Naohiro Takemoto and co-workers from Kyoto University for their work showing that “coaggregates” of pancreatic islets and regulatoryT cells resulted in improved transplant outcomes in experimental models of islet transplantation.
Donna Lucas, et al
The Anthony P. Monaco Award that recognizes the best translational submission went to Donna Lucas and co-workers from Johns Hopkins University for their clinical study investigating antibody responses in renal patients across different MHC mismatches, with the aim of improving donor-patient matching and to better apply immunosuppression
Both the Leslie Brent and the Anthony P. Monaco awards are wonderful opportunities to highlight outstanding publications in Transplantation. We are presently looking forward to reviewing the best submissions of 2016 and will accept applications until June 30th, 2017.
- Asian Society of Transplantation (AST)
- Asociacion Guatemalteca de Nefrologia
- Associacao Brasileira de Transplante de Orgaos (ABTO)
- Asociacion Colombiana de Trasplantes de Organos (ACTO)
- Austrotransplant
- Belgian Transplantation Society (BTS)
- British Transplantation Society (BTS)
- Canadian Society of Transplantation/
- Société canadienne de transplantation (CST)
- Croatian Society of Transplantation Medicine (CSTM)
- Deutschen Transplantationsgesellschaft
- International Transplant Nurses Society (ITNS)
- Hong Kong Society of Transplantation (HKST)
- Nederlandse Transplantatie Vereniging (NTV)
- Regional Health Development Center (RHDC)
- Croatia on Organ Donation and Transplant Medicine
- Sociedad Argentina de Trasplantes (SAT)
- Sociedad Chilena de Trasplante
- Sociedad Espanola de Trasplante (SET)
- Sociedad Mexicana de Trasplantes (SMT)
- Società Italiana Trapianti d'Organo (SITO)
- Societat Catalana de Trasplantament (SCT)
- Southern African Transplantation Society (SATS)
- The Japan Society for Transplantation (JST)
- The Korean Society for Transplantation
- The Middle East Society for Organd Transplantation (MESOT)
- The Swedish Transplantation Society
- Swisstransplant Society (STS)
- Thai Transplantation Society
- Transplant Society of Pakistan
- Transplantation Society of Australia and New Zealand (TSANZ)
- Turkic World Transplantation Society (TDTD)
- Turkish Transplantation Centers Coordination Association
- Turkish Transplantation Society (TOND)
- Urologic Society for Transplantation and Renal Surgery
For more information on these and all of our affiliates, please visit the Affiliated Societies page on the TTS website.
This Guide contains the most updated information and guidance for all professionals involved in identifying possible organ donors, coordinators managing the process of donation after death and of living donation, professionals responsible for the allocation and clinical use of human organs, quality managers and Health Authorities responsible for overseeing donation and transplantation programmes.
In this 6th Edition, all of the chapters have been revised thoroughly to update their contents with the most recent advances in the field. In addition, new and important chapters have been added, including specific guidance for the determination of death by neurologic criteria, donation after circulatory death and living donation, among others.
This Guide constitutes a common European standard, based on the long-standing expertise and knowledge of the European Directorate for the Quality of Medicines & Health Care (EDQM), Council of Europe.
The electronic version of this Guide is available for free download at EDQM’s dedicated website after a simple registration process. Paper copies are available for purchase at the EDQM Store.
The Lancet Kidney Campaign was launched on March 10, 2016 to mark World Kidney Day (WKD). Initiated by The Lancet and the International Society of Nephrology (ISN), this Campaign is joined now by TTS and other leading global kidney organisations around the world to keep clinicians, policy-makers and collective societies in regions throughout the world informed with research, expert commentaries and analysis on acute kidney injury (AKI), chronic kidney disease (CKD), dialysis and transplantation from across the journal's database.
The Campaign also provides regular updates on recent advances in nephrology, as well as expert commentaries and interviews on key health and policy issues relevant to kidney disease. The most recent updates include:
- The ISN Global Kidney Health Summit: Setting a blueprint for tackling global CKD epidemic
- Kidney disease in Indigenous populations
- Obesity and overweight populations in Latin America
- Ramadan and chronic kidney disease patients
We invite you to visit the Lancet Kidney Campaign website and explore its in-depth and up-to-date resources.
The Advanced Renal Transplantation Webinar Series continues for the second year: The series consists of 24 monthly webinars presented by world-class leaders from the international transplant community in their respective disciplines. Please visit the series page for more information. A similar series in liver transplantation is in preparation and more information will be posted online soon.
For the recent Congress in Hong Kong, the Education Committee participated in the organization of the post-graduate education (PGE) course, which included a balanced clinical and basic science program. Expanded
info about the course remains available on the TTS 2016 website.
In addition to the sciences, the Education Committee has been experimenting with non-traditional topics and format for delivering continuing education and professional development content. With this in mind, the Education Committee sponsored two very exciting morning symposia at the 2016 TTS Congress, the first of which was entitled “Fostering Innovation To Avoid Extinction: Current Trends in Health Professions Education”. With presentations given by healthcare education professional experts, this symposium highlighted the gap between current needs for training transplant professionals and skill levels among transplant professionals, and presented strategies and models to bridge this gap. Expanded info about this symposium remains available on the TTS 2016 website.
The second symposium was entitled “Establishing Immunogenetics & Transplantation Laboratories & Implementing Newer Technologies”, which included short presentations and interactive discussions about starting up transplant immunology laboratories and introducing new testing technologies. This session was designed with a mindset that establishing best practices in transplant immunology across the world requires both deep understanding of the unique challenges that face different parts of the world and building on the experiences of well-established labs and international histocompatibility professional societies. The symposium highlighted success stories in establishing transplant immunology laboratories and implementation of newer technologies in India, Pakistan and Korea. These presentations were followed by interactive small group discussions. Expanded info about this symposium remains available on the TTS 2016 website.
Recordings of the sessions referred to in this article are accessible through the Education portal on the TTS website at www.tts.org/education.


The Society has great educational tools on its website and we want to do more. Please keep an eye out for some new updates from our Young Members Committee. Plans include adding a section with job postings, opportunities to travel, and expand leadership skills. We will also be launching a section on how to career plan, which will include advice from many mentors in TTS.
In these last few months some of you took part in our survey and we have listened to your answers:
Networking and communication between young clinicians and scientists, as well as between young and senior members of TTS is very important. At the TTS Congress in Hong Kong, a Young Investigator event supported by Gift of Life was held at The Pawn. The idea was to give young people the opportunity to get to know each other and also to socialise with senior members of the society. The event was very successful and we hope to have several similar events in 2017.
Social media is important and we are currently setting up several platforms for the TTS Young members.
It is our aim to contact you in many different ways – we hope to see you at some of the Section meetings’ networking events in 2017!


with the 10th Anniversary of the Declaration in 2017, the Custodian Group is focused on updating its definitions and and engaged with world leaders
The Declaration of Istanbul Custodian group (DICG) is currently concentrating on two main focus areas:
- Education to medical practitioners working in the field of transplantation to understand the principles of organ trafficking and commercialism;
- Education to Governments and Departments of Health to understand the need for their intervention to prevent these unethical practices.
In this regard the workshop that was held in April 2016 in Madrid, highlighted some of the ongoing problems professionals are still seeing: living donor exploitation by commercialism, poor consent-taking practices and inadequate medical and follow-up care. This remains a pressing problem in many parts of the world and is often flagged by clinicians who look after patients who travel for a transplant. These patients would go to countries where the illegal organ trade is possible, mainly because they have poor regulation, lack of oversight and inadequate vigilance, surveillance and guidelines. Because organ trade is mostly presented as a criminal offense in need of a punitive response, countries that are unable to provide the necessary response are usually a target for organ traffic networks. Because of this issue, organ trafficking often goes hand-in-hand with patients traveling: the donor, the recipient or both patients might travel to supply an organ or receive a transplant in another country.
The DICG is currently planning the 10th Anniversary Meeting of the Declaration of Istanbul (DOI) with a meeting for the working groups in June 2017. During the next two years, the DOI will be updated in terms of definitions and structure in order to accommodate some of the new issues we are facing.
DICG is currently actively engaging with the World Health Organization, governmental leaders, religious leaders as well as lawyers and chief justices to combat organ trafficking with appropriate legal and professional responses. There is currently constant engagement with ministers of health, specifically Mexico, India, Egypt and Turkey.


The Women in Transplantation Initiative held two exciting educational events for women transplant professionals at the TTS 2016 Congress in Hong Kong. The highly successful WIT Workshop and Networking Cocktail, chaired by Professor Nancy Ascher, featured career development seminars by Dr. Megan Sykes, the Michael J. Friedlander Professor of Medicine at Columbia University; Imke de Lanversin, of Novartis Global; and, Mayumi Chida, of Novartis Japan. The expert panel provided key insights into how to position yourself to achieve your career goals.
The WIT Scientific Symposium, chaired by Professor Lori West and Professor Ascher, featured two innovative talks focused on Sex and Gender in Transplantation. Dr. Nithya Krishnan, a consultant transplant nephrologist at University Hospitals Coventry, UK, kicked off the session discussing her research study entitled “Are Women in Transplant Leadership Roles Judged More Harshly than their Male Colleagues?” Dr. Cara Tannenbaum, Scientific Director of the Institute of Gender and Health at the Canadian Institutes of Health Research, provided a stimulating and thought-provoking lecture on “Why Sex and Gender Matter in Transplantation Research”.
In addition to these events, and based on WIT input into the scientific program content, Dr. Kathryn Tinckam gave an excellent talk entitled “Biologic Impact of Gender/Sex on Outcomes of Transplantation and Living Donation”.
WIT would also like to congratulate the 2016 Women in Transplantation Award recipients. Dr. Lori West received the Women Leader in Transplantation Award and Dr. Elmi Mueller and Mrs. Lalitha Raghuram
were co-recipients of the WIT Hero Award. (see 2016 Women in Transplantation Awards).
Two recent autumn WIT events kept with the theme of “Sex and Gender in Transplantation”. The WIT Networking Breakfast at the ASHI Annual Meeting was held on September 29th, in St. Louis. Dr. Lori West presented Dr. Tannenbaum’s talk to a large and highly engaged audience, covering clinical, scientific and policy as well as career aspects of the topic.
Paving the way toward future collaboration, on October 14th, in Pittsburgh, WIT held a Networking Cocktail during the International Transplantation Nurses Society Symposium. Moderated by Sabina De Geest, once again the event was very well-attended and active. Guest speakers Nancy L. Stitt and Kandy Yarris Newell presented “Turning Vision into Reality - A Story of the History and Future of ITNS”, followed by speaker Sandra Couples who briefly presented on the future focus of ITNS and continued partnerships, which included TTS and WIT. TTS IHQ Membership Coordinator, Amanda Mayer, spoke on behalf of WIT, touching on the origins and goals of the Initiative, and how to become a WIT member.
We are also pleased to report on the success of the first WIT Round Table dinner meeting on October 13, 2016 in Los Angeles supported by Novartis. This inaugural WIT dinner event was attended by over 45 women and men transplant professionals from Los Angeles, many of whom had never attended a WIT educational event before. Moderated by Alyson Huff from Novartis, the event featured Dr. Elaine Reed, UCLA Professor of Pathology, and participants engaged in a lively discussion on how transplant professionals can increase awareness of sex and gender issues in Science and Medicine.



The Cell Transplant and Regenerative Medicine Society (CTRMS) under its expanded vision to embrace members with an interest in regenerative therapies, enters its second year under its new name. The Society has welcomed new members and is launching new initiatives to achieve its mission. There are now three active committees: the Social Media and Web Committee, Membership Committee and Young Investigators Committee. The CTRMS is actively seeking new members to lead in the fields of mesenchymal stromal cells, neuronal regeneration, islet cells, muscle, cartilage, bone, cardiac and lungs and colleagues from tissue engineering.
CTRMS members who have a wealth of experience in using cellular therapies in organ failure could provide assistance to researchers in the field of stem cells and regenerative therapies to facilitate their translation into clinical practice. We would like to invite you to become a member of our Society, and join us in Halifax, Nova Scotia, Canada, for our joint meeting with the Canadian Society of Transplantation taking place on September 26-29, 2017.
The IPITA is just back from Boston, where we held a high-profile key opinion leader meeting on Stem cell-derived beta cells. The meeting took place at Harvard Medical School from September 18-20, and was jointly organized by IPITA, JDRF, the Helmsley Charitable Trust and the Harvard Stem Cell Institute. Jon Odorico and James Markman, the current President and Secretary of IPITA, designed an intense scientific program; twenty-nine invited speakers addressed the two-day meeting, which was attended by 75 invited participants, including 4 young investigators awarded with a competitive travel grant.
The sessions comprised of invited lectures and panel discussions on a variety of topics related to stem cell therapy for type 1 diabetes. After a kick-off state-of-the-art session on beta cell differentiation, topics including functional assessment, genetic engineering and its hazards, immune responses, and transplant sites were addressed during the first day. On the second day, encapsulation technologies and animal models were discussed, before concluding the meeting with two sessions reviewing the regulatory issues and clinical targets.
The meeting comprehensively covered all aspects, issues, tools and perspectives of stem-cell derived therapy for type 1 diabetes. The high standard of the invited lectures was matched by the very active participation of the delegates and the lively and in-depth discussions between the floor and the podium. The meeting brilliantly succeeded in bringing together a wide spectrum of stakeholders in the field and in providing a unique forum for exchanging ideas and fostering collaboration. Recordings of many of the presentations will son be available to IPITA and TTS members on the IPITA website.

The next IPITA endeavour will be a workshop on definitions of outcomes and success criteria in beta cell replacement therapies. These are critical issues requiring long overdue discussions. The workshop will take place in Igls, Austria on January 28-29, 2017 and will be organized in partnership with EPITA, the European Pancreas and Islet Transplant Association, just before their annual Winter Symposium. The program is being finalized by a committee under the leadership of Michael Rickels, IPITA Councillor. Please visit the Symposium website for more information.
Finally, the IPITA will hold its 16th International Congress in Oxford from June 20-23, 2017. The Congress chairs Paul Johnson and Peter Friend are making sure that cutting-edge science and congenial networking will be offered to participants in this attractive venue.
These programmed events continue to demonstrate that IPITA is a vibrant and thriving Association committed to offering outstanding value to its membership. IPITA looks forward to seeing you in Igls and Oxford!
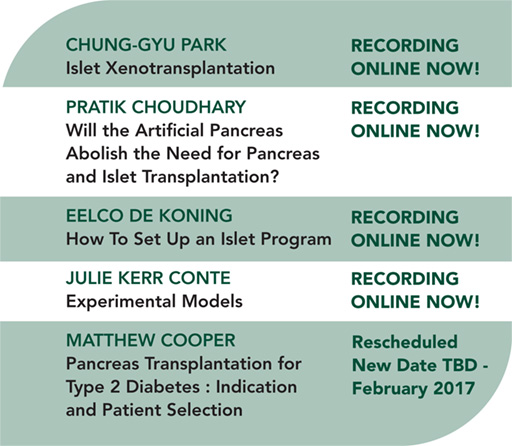
We are in the process of building content for our 2017 series. For questions, comments or ideas, please contact our webinar coordinators Thierry Berney or Barbara Ludwig at info@TTS.org.

The Executive Committee and Council of the International Pediatric Transplant Association (IPTA) are pleased to provide an update of our Association's activities.
Education Committee Update
Chair: Christian Benden, switzerland
Incoming Chair: Rohit Kohli, USA
The Education Committee has continued in 2016 to expand the Society’s educational activities co-organizing the biennial IPTA Fellows Symposium on Pediatric Transplantation that took place at Mount Sinai in New York City in April this year with 30 fellows from around the world and an international faculty of experts in the field of pediatric transplantation. The IPTA Fellows Symposium provided updates in a broad spectrum of pediatric transplantation, but furthermore, an ideal environment for networking and mentoring. The Education Committee successfully submitted symposium proposals for the American Transplant Congress in May 2016 in Boston, MA, USA, and contributed to the educational content of a Joint IPTA/TTS Pediatric Post Graduate Course at the 26th International Congress of The Transplantation Society in August 2016 in Hong Kong.
Infectious Disease Care Committee Update
Chair: Upton Allen, Canada
The focus of the ID-CARE initiative is ID Clinical Care, Advocacy, Research and Education. The Committee seeks to engage IPTA members from all disciplines within pediatric organ and stem cell transplantation. The ID CARE Committee has been involved in several initiatives, some of which have been published in Pediatric Transplantation (curriculum-related documents). In keeping with this approach, the group is currently working on a document that focuses on the evaluation and management of transplant candidates or recipients with recent active infections (authors Arnaud L’Huillier, Upton Allen and Michael Green). The group has also identified the following projects which are at varying stages of completion:
- Status of Use of Live Vaccines After Pediatric
Solid Organ
Chair: Klara Pofsay-Barbe - Pneumocystis Prophylaxis Strategies Across Transplant Centers
Chair: Mignon McCulloch and Marian Michaels - Tuberculosis and Transplantation:
A Pediatric Perspective
Chair: Mignon McCulloch
9th Congress of IPTA
Barcelona, Spain, May 27-30, 2017
Chair: Anne I. Dipchand, CANADA
Program planning is well underway and we are thrilled with the response and enthusiasm of our invited speakers! Look for the preliminary program online. Collaboration is an important part of the IPTA 2017 Congress. On the springboard of our partnership with TTS, we have actively pursued opportunities to partner with other transplant organizations. It is important that we all work together as a community to advance the science and practice of transplant medicine, especially the pediatric component through IPTA. The Barcelona Congress will showcase collaborative sessions between IPTA and the following organizations: American Society for Histocompatibility & Immunogenetics (ASHI); American Society of Transplantation (AST), American Society of Transplant Surgeons (ASTS).


The ISODP Council in conjunction with the TTS Leadership recently hosted a highly successful Leadership Workshop on Organ Donation and Transplantation in Beijing, China. Building on the well-received 2015 workshop in Riyadh, Saudi Arabia, this program continued focus on the ISODP’s strategic goals of:
1) Increasing donation worldwide
2) Improving scientific knowledge
3) Growing community involvement
The ISODP, TTS, the China Organ Donation and Transplant Committee and other hosts brought together global experts for a program focused on strategic, structural and operational activities to develop effective and high performing organ donation programs. Conference Chairs Marti Manylich, ISODP President and Jiefu Huang, Director China Organ Donation and Transplantation Committee along with TTS President Nancy Ascher framed the workshop with the highest expectations to provide resources and support to the developing Chinese organ donation programs in the new era of donation and transplantation. Scientific Committee Chairs Kimberly Young, ISODP Past President, and Haibo Wang, ISODP Councilor, convened an international panel of experts from eight nations and the WHO who shared global highlights and challenges.
For the 80 key donation professionals from across China the workshop provided a platform for growth as China works to improve donation practices and results. Engaged dialogue and sharing stimulated new initiative and inspiration for all participants. ISODP will continue its focus on providing support to developing programs and is pleased to be collaboration with China at this time of great opportunity.
The Society is also pleased to promote the 14th ISODP Congress to be hosted in Geneva, Switzerland from September 5-9, 2017. The Scientific Committee is developing a robust and exciting agenda focused on innovation and emerging best practices. Importantly the Congress will be held in conjunction with the World Donation Day and the European Donation Day. Make plans to join us in Geneva!

Under the auspices of the ISVCA and with the support of TTS, the Second International Chauvet Workshop was held in Paris from September 17-20, 2016. Attendees came from countries around the world including centers from Europe (Austria, France, Italy, Poland, Sweden), USA, Mexico, Turkey, India, Australia, and representing the majority of teams involved in upper extremity (14 teams), face (6 teams) and uterus (2 teams) transplantations.
The second workshop built upon the success of the first Chauvet Workshop by creating a platform for the open and collegial discussion regarding psychosocial and ethical issues in VCA, including upper extremity, face and uterus transplantations.
During the first Chauvet workshop, the attendees highlighted the domains of importance in the psychosocial assessment and management of upper extremity transplanted patients and the need for an international consensus on them. One of the goals of the second workshop was to create a set of “recommendations” on the basis of a survey sent to all active centers. The results of the survey were presented and discussed during the workshop.
An update on the psychosocial issues in face transplantation was followed by an in-depth discussion organized around four roundtables on critical topics in face transplantation including: suicide and face transplantation, body image, psychological follow-up and support of the face grafted patients and ethical issues. These discussions aimed at defining the patient selection process and candidate eligibility, establishing the risk/benefit balance, determining the patients’ ability to understand risk and describing the optimal follow-up of face grafted patients.
Uterus transplantation is an emerging area within VCA with unique psychosocial and ethical issues, which were presented by the teams currently involved in this type of transplantation. This presentation was enhanced by the participation of transplant ethicists who considered the possible benefits and risks for this patient population.

The 2015 Xeno-Prize was judged recently and we are pleased to announce that the winner is Dr. Leela Paris for her paper entitled: “Reduced human platelet uptake by pig livers deficient in the asialoglycoprotein receptor 1 protein”. Congratulations to Dr. Paris and her co-authors for their outstanding work.
It is our great pleasure to invite you to the next Congress of the International Xenotransplantation Association (IXA) in Baltimore, USA, September 20-23, 2017. Baltimore is a popular tourist destination, conveniently located at proximity to other major cities on the East coast. The venue for the meeting is on the University of Maryland Baltimore’s campus, located close to the Inner Harbor in downtown Baltimore. The University of Maryland Southern Management Center (SMC) provides an amazing location for this event. Adjacent to Camden Yards, the Baltimore Orioles’ home field, SMC is a modern, convenient and flexible facility well-suited to host our Congress. Social events will take advantage of local cultural and architectural landmarks, most within walking distance of the campus and convenient meeting hotels.
The Scientific Program Committee is designing an exciting program to meet and discuss innovative strategies for overcoming immunologic, technologic, regulatory and other obstacles to xenotransplantation. Young investigators are invited to submit their work for oral and poster presentations, in order to make this meeting a vibrant and productive platform for scientific exchange and discussion. For more information on the meeting, please visit www.ixa2017.org.
The IXA Congress will be held in conjunction with pre-symposium focused on strategies for the management of hyper-immunized and ABO-incompatible organ allograft recipients, and will be followed by the Swine in Biomedical Research meeting, attracting a constituency whose scientific and technical interests overlap substantially with those of IXA.
The IXA Council has initiated a discussion with the FDA to discuss existing guidelines for clinical xenotransplantation and is inviting all IXA members to actively participate by sending questions or comments to sections@tts.org.
As the year is ending, don’t forget to submit your manuscript to Xenotransplantation for a chance to win the 2016 Xeno-Prize, and to make your donation to the Reemtsma Lectureship Fund.

As reported previously in the Tribune, the endorsement by the IRTA membership for the change in the name of our Association took place at the 2015 Congress in Buenos Aires, Argentina. The new name more accurately reflects the commitment of our Association to multidisciplinary education and research along the entire continuum of care for patients with intestinal failure. We are now actively planning the next meeting of IRTA and we ask that you mark your calendars, prepare your most significant observations and discoveries for abstract and poster presentations and plan to attend the Congress of the Intestinal Rehabilitation and Transplant Association (CIRTA 2017) in New York City June 28 – July 1, 2017. Please visit the Congress website for more information about the exciting program that is planned.
The morning air is crisp signifying the welcomed transition of the season from summer to fall. Like the change of seasons (and in addition to the name change), our Association is undergoing a subtle, but no less profound transformation. One of the signature functions of our Association has long been the summary of the world experience in intestinal transplantation at our biennial international small bowel transplant symposium. The International Intestinal Transplant Registry (IITR), which was founded by David Grant and until now managed at the University of Toronto, has been the repository for the data that informed these updates. As intestinal transplant volume has grown and our Association has matured, Dr. Grant encouraged the transition of responsibility for the Registry to the Scientific Committee of our Association. The Council agreed and examined several proposals for this transition to a new and sustainable location and structure. We are proud to announce a new partnership between the IRTA and the Terasaki Institute for the maintenance of the historic functions of the Registry. In addition, the IITR is also now positioned to become a platform that may support multicenter trials, collaborations and innovation in order to move the field forward.
As we gain momentum with these transitions, we anticipate more substantial collaborations that will undoubtedly lead to new discoveries that are not possible from the observations of single center small case series. This is an exciting time for our Association and we look forward to seeing you in New York next year!
The Transplant Infectious Diseases Section hosted a great meeting on August 18, 2016 in Hong Kong, one day prior to the start of TTS 2016. The meeting featured speakers from five continents, with talks highlighting topics such as hepatitis B and C infection, multidrug resistant organisms, and emerging arboviruses such as Zika and Dengue. We also heard expert presentations about CMV, novel herpes viruses, challenging respiratory viruses, and the current antiviral pipeline. The one-day Congress featured a session with challenging cases presented by all speakers, followed by a delicious dinner at Hullet House. The TID Section is now planning our next annual meeting to be held in Montevideo, Uruguay on September 25, 2017, one day prior to the start of the STALYC Congress. TID 2017 will include presentations in English with simultaneous translation available in Spanish to all attendees. Admission to this educational meeting is not restricted to infectious disease specialists, and as in past meetings we expect to welcome many other interested transplant professionals.
The TID Section has an active e-mail listserv, TIDChat, to which members are free to post clinical questions to our international membership. Challenging topics are discussed and recommendations shared in an open and interactive forum. TID membership also includes digital access to the section journal Transplant Infectious Diseases on computers, tablets, and mobile phones. The TID Section will be hosting webinars in the coming year, and is also working with several organ-specific transplant associations to host joint symposia at their upcoming annual conferences. TID membership is open to all practitioners with an interest in the infectious complications of transplantation. In addition, our Section would be glad to collaborate with other TTS groups to improve transplant outcomes by promoting a better understanding of transplant infection management.
To consolidate its position as the leading global organization, the Council has representation from all six regions of the world: Asia, Europe, Latin America, Middle East/Africa, North America and Oceania.
EXECUTIVE MEMBERS
| PRESIDENT Nancy Ascher |
| PRESIDENT-ELECT Mehmet Haberal |
| IMMEDIATE PAST PRESIDENT Philip J. O’Connell |
| VICE-PRESIDENT Marcelo Cantarovich |
| SECRETARY John J. Fung |
| SENIOR TREASURER Elmi Muller |
| TREASURER Stefan G. Tullius |
| HISTORIAN Randall E. Morris |
| INTERNATIONAL HEADQUARTERS Jean-Pierre Mongeau Executive Director |
COUNCILORS
| ASIA Hiroto Egawa Jongwon Ha S. Adibul Hasan Rizvi |
| EUROPE Beatriz Domínguez-Gil Peter J. Friend |
| LATIN AMERICA Gabriel E. Gondolesi Alejandro Niño Murcia |
| MIDDLE EAST / AFRICA Ifeoma Ulasi |
| NORTH AMERICA Medhat Askar Minnie Sarwal Peter G. Stock |
| OCEANIA Steven J. Chadban |
Tribune is published by
The Transplantation Society (TTS).
Editor-in-Chief: Nancy K. Man
International Headquarters
International Headquarters
The Transplantation Society
505 boul. René-Lévesque Ouest
Suite 1401
Montreal, QC H2Z 1Y7 CANADA
T. +1.514.874.1717
F. +1.514.874.1716
E. info@tts.org
W. www.tts.org
Please contact any of our dedicated staff for any assistance you may require:
| Roman Beliaevski IT/Multimedia roman.beliaevski@tts.org |
| Roberto Colarusso Director of Technologies robert.colarusso@tts.org |
| Geneviève Leclerc Director of Meetings genevieve.leclerc@tts.org |
| Sondra Livingston Sections Manager sondra.livingston@tts.org |
| Amanda Mayer Membership Services Coordinator amanda.mayer@tts.org |
| Jean-Pierre Mongeau Executive Director jp.mongeau@tts.org |
| Catherin Parker Meetings Manager catherin.parker@tts.org |
| Chelsea Patriquin Meetings Coordinator chelsea.patriquin@tts.org |
| Denise Rainville Controller denise.rainville@tts.org |
| Eugenia Siu Registration & Administration Coordinator eugenia.siu@tts.org |
| Darren Woodbury Graphic Designer darren.woodbury@tts.org |
| Chi Hong Yeung Accounting Clerk chihong.yeung@tts.org |
Contact
Address
The Transplantation Society
International Headquarters
740 Notre-Dame Ouest
Suite 1245
Montréal, QC, H3C 3X6
Canada
Используйте Вавада казино для игры с бонусом — активируйте промокод и начните выигрывать уже сегодня!