2017 - IPITA
This page contains exclusive content for the member of the following sections: TTS, IPITA. Log in to view.
Pancreas Transplantation - Outcomes & Complications 1
5.3 - Influence of the Procurement Team on Pancreas Transplant Outcomes.
Presenter: OK, Serrano, Minneapolis, United States
Authors: Oscar Serrano, David Vock, Ty Dunn, Raja Kandaswamy, Erik Finger
Influence of the Procurement Team on Pancreas Transplant Outcomes.
O. Serrano1, D. Vock2, T. Dunn1, R. Kandaswamy1, E. Finger1.
1Surgery, University of Minnesota, Minneapolis, MN,USA, ; 2Biostatistics, University of Minnesota, Minneapolis, MN,USA,
Objective: A number of single center studies have demonstrated utility of regional organ procurement collaboration to reduce travel redundancy by procuring surgical teams with no difference in transplanted organ outcomes for a variety of abdominal organs. We sought to determine if the procuring surgeon had an effect on pancreas transplant outcomes.
Methods: We studied outcomes for pancreas allograft recipients from deceased donors transplanted between January 1, 2002 and December 31, 2014 using the Scientific Registry of Transplant Recipients (SRTR). We compared outcomes between organs procured by the recipient’s center (transplant procurement team; TPT) versus non-TPT (NTPT). To assess the effect of TPT on graft survival (GS), death-censored graft survival (DCGS), and overall survival (OS), we fit a mixed-effect Cox proportional hazards model adjusting for procurement team, recipient and donor demographics, and surgical technique. Transplant center and volume was included as a random effect in the model.
Results: Between 2002 and 2014, there were 4,181 pancreas alone (PAT; 38.2% TPT) and 9,423 kidney-pancreas (KP; 57.2% TPT) transplants. On multivariate analysis, longer cold ischemia time (p<0.001); increasing donor age (p<0.001) and black race (p=0.01); increasing recipient age (p<0.001), increasing BMI (p<0.001), and worse functional status (p=0.02) were associated with worse DCGS. When compared to NTPT, GS for organs procured by TPT was significantly better for KP (0.88; 0.81-0.96), but not for PAT (1.05; 0.95 -1.17). Adjusted 3-year DCGS comparing TPT to NTPT was 81.9% vs 80.2% (p<0.001) for KP; 83.4% vs 80.6% (p=0.047) for PAT. DCGS was significantly better comparing TPT to NTPT for KP but not PAT (Figure 1), while OS was not significantly distinct among the procurement cohorts (Table 1).
Conclusion: Our findings contradict previous support for regional organ procurement collaboration in pancreas transplantation. The economic and personnel investment TPT devote to procuring their own organs may be justified for KP but not PAT.
Table 1. Adjusted HR comparing grafts procured by a team from the recipient’s center to all other grafts adjusting for recipient and donor factors.
KP
PAT
DCGS
0.87 (0.79 - 0.97)
0.99 (0.88 - 1.12)
GS
0.88 (0.81 - 0.96)
1.05 (0.95 - 1.17)
OS
0.88 (0.78 - 0.99)
1.18 (0.99 - 1.40)
Figure 1. Death-Censored Graft Survival for Simultaneous Kidney Pancreas Transplants.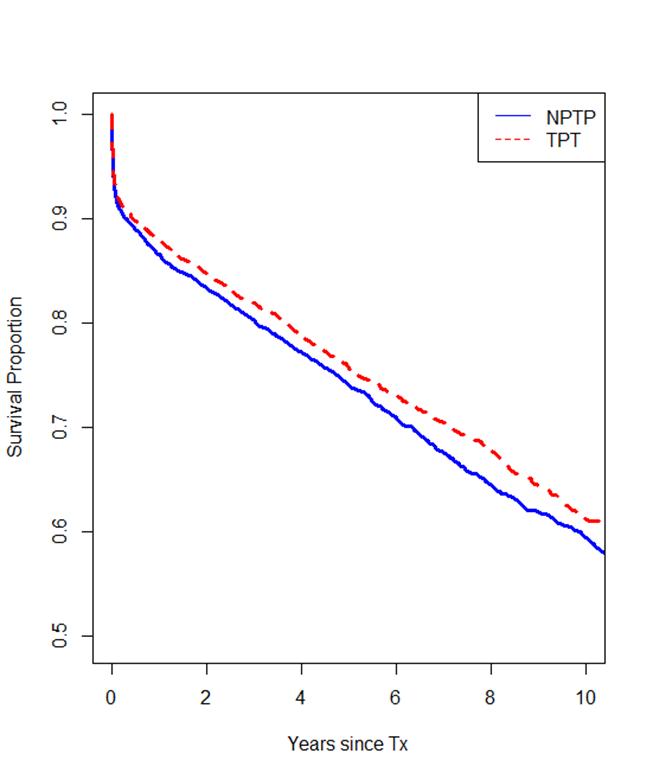
Important Disclaimer
By viewing the material on this site you understand and accept that:
- The opinions and statements expressed on this site reflect the views of the author or authors and do not necessarily reflect those of The Transplantation Society and/or its Sections.
- The hosting of material on The Transplantation Society site does not signify endorsement of this material by The Transplantation Society and/or its Sections.
- The material is solely for educational purposes for qualified health care professionals.
- The Transplantation Society and/or its Sections are not liable for any decision made or action taken based on the information contained in the material on this site.
- The information cannot be used as a substitute for professional care.
- The information does not represent a standard of care.
- No physician-patient relationship is being established.
Contact
Address
The Transplantation Society
International Headquarters
740 Notre-Dame Ouest
Suite 1245
Montréal, QC, H3C 3X6
Canada
Используйте Вавада казино для игры с бонусом — активируйте промокод и начните выигрывать уже сегодня!
