2011 - BSS 2011 Symposium
This page contains exclusive content for the member of the following sections: TTS. Log in to view.
Oral Presentations 2
11.2 - Tubular atrophy and interstitial fibrosis following renal transplantation is dependent on galectin-3.
Presenter: Lorna, Marson, Edinburgh, United Kingdom
Authors: Lorna Marson1,2, Zexu Dang1, Alison MacKinnon1, Tariq Sethi1
Tubular atrophy and interstitial fibrosis following renal transplantation is dependent on galectin-3.
Lorna Marson1,2, Zexu Dang1, Alison MacKinnon1, Tariq Sethi1
1Centre for Inflammation Research, University of Edinburgh; 2Transplant Unit, Royal Infirmary of Edinburgh; Edinburgh, UK
Chronic allograft injury, characterised by interstitial fibrosis and tubular atrophy, is a significant challenge in renal transplantation, leading to progressive decline in function over months and years. It results in the loss of 5% of renal transplants per annum and currently eludes specific therapies. Galectin-3 is a β-galactoside- binding lectin that is highly expressed in fibrotic tissue of diverse aetiologies, and mice deficient in galectin-3 have reduced fibrosis in a range of organs, including kidney, liver and lung. The role of galectin-3 in the development of chronic allograft injury is examined in this study.
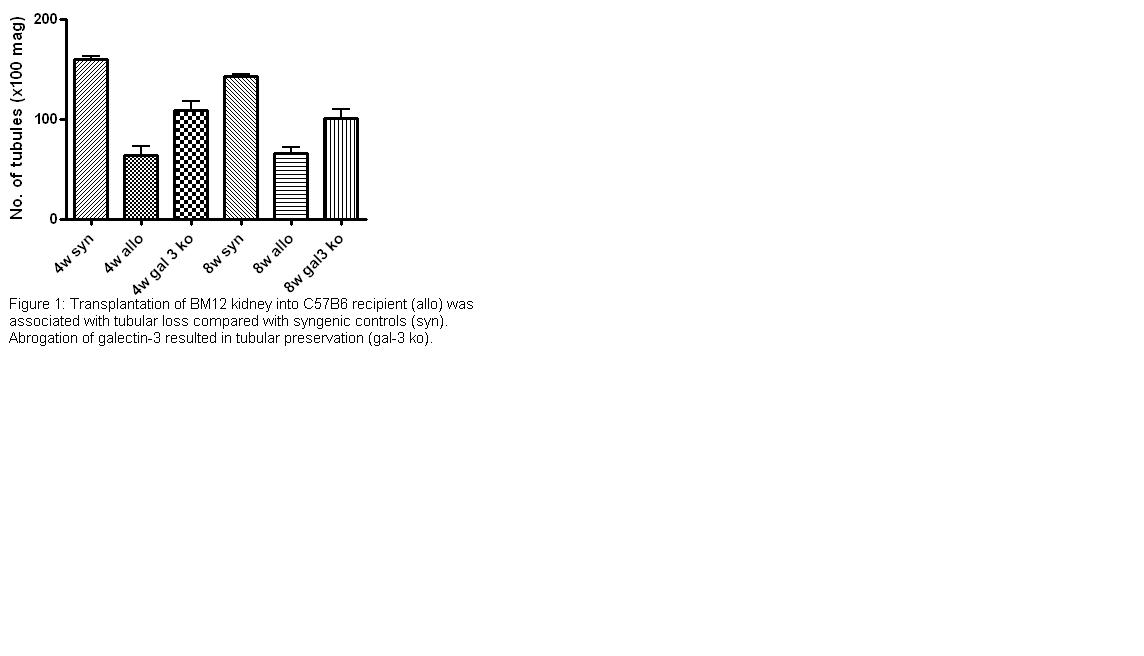
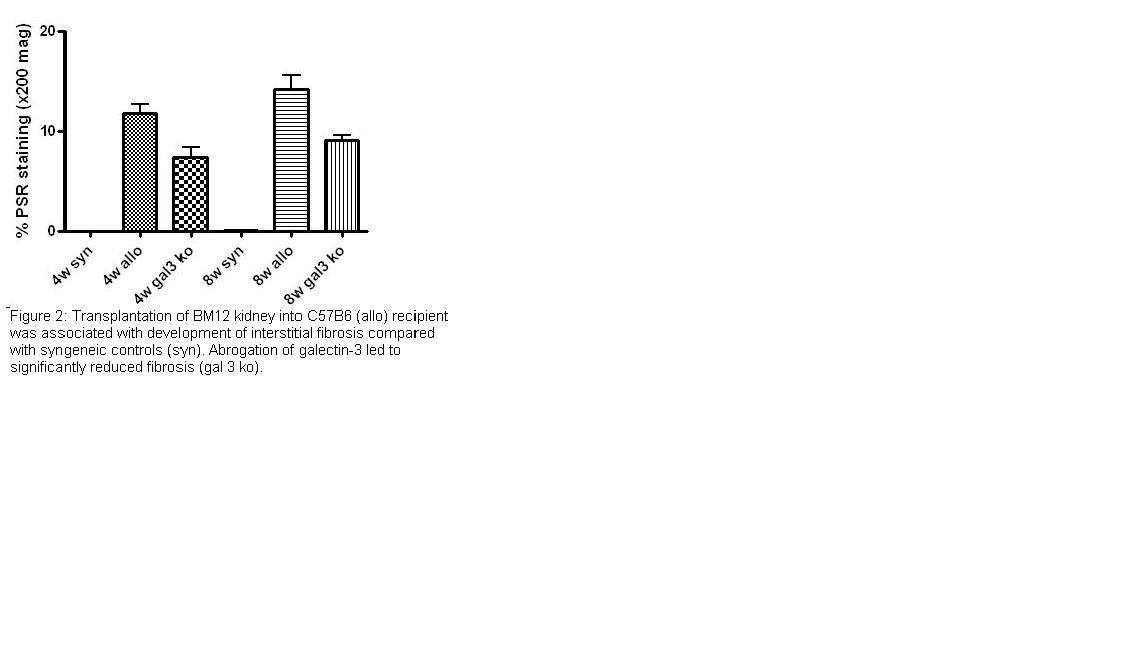
We adopted a murine model of chronic allograft injury, characterised by a single class II mismatch between BM12 donor and C57B6 recipient strains. This was associated with the development of interstitial fibrosis (p<0.0001) and tubular atrophy (p<0.0001) at 4 weeks, and marked upregulation in galectin-3 expression (p=0.002), compared with syngeneic (C57B6) control transplants.
Transplantation of BM12 kidneys into galectin-3 null mice on a C57B6 background resulted in significant preservation of tubules (p=0.008), shown in Figure 1, and reduced interstitial fibrosis (p=0.01), as shown in Figure 2. This was associated with decreased myofibroblast activation (p=0.01) and collagen I (p=0.04) expression, compared with wild type controls at 4 weeks. The number of infiltrating leucocytes (T and B cells, and macrophages) was unaltered by abrogation of galectin-3, but reduced expression of ym1 (p=0.0001), a marker of alternative macrophage activation, in the galectin-3 null mice suggests a possible mechanism by which galectin-3 promotes renal transplant fibrosis. Our results suggest that galectin-3 plays a central role in the development of interstitial fibrosis and tubular atrophy in the context of chronic allograft injury and provides a potentially exciting therapeutic target.
Important Disclaimer
By viewing the material on this site you understand and accept that:
- The opinions and statements expressed on this site reflect the views of the author or authors and do not necessarily reflect those of The Transplantation Society and/or its Sections.
- The hosting of material on The Transplantation Society site does not signify endorsement of this material by The Transplantation Society and/or its Sections.
- The material is solely for educational purposes for qualified health care professionals.
- The Transplantation Society and/or its Sections are not liable for any decision made or action taken based on the information contained in the material on this site.
- The information cannot be used as a substitute for professional care.
- The information does not represent a standard of care.
- No physician-patient relationship is being established.
Contact
Address
The Transplantation Society
International Headquarters
740 Notre-Dame Ouest
Suite 1245
Montréal, QC, H3C 3X6
Canada