TTS Masterclass Series Announcement
TTS Members can now register for FREE for the last two Masterclass Series on Transplant Immunology and Outcome Reporting. Members must pre-register to attend the live Masterclasses.

TTS is pleased to announce that the remaining two Masterclass Series (Transplant Immunology Series & Outcome Reporting Series) have been granted European CME credits (ECMEC®s) by the European Accreditation Council for Continuing Medical Education (EACCME®).
Attendance at the live Masterclasses is mandatory to receive the certificate.

Online First Highlighted Articles
Highlighted Tweets
Updated Statement About Vaccine Efficacy in Transplant Recipients
UPDATED JOINT AST/ASTS/ISHLT STATEMENT ABOUT VACCINE EFFICACY
IN ORGAN TRANSPLANT RECIPIENTS.
Community spread of SARS-CoV-2 is waning in some parts of the world, especially in those areas with greater vaccine acceptance. Information about COVID-19 vaccine responses in transplantation is rapidly evolving. The impact of more easily transmissible variants is unknown but is likely to be less where greater numbers of individuals are vaccinated. Because vaccines are critical to containing further spread of the pandemic, there has been interest in optimizing vaccine responses in vulnerable populations, including solid organ transplant (SOT) recipients. To date, we have learned the following:
- Antibody responses to COVID-19 vaccines in transplant recipients are diminished compared with the general population (1-14). However;
- The level of protective antibody has yet to be defined. Based on data derived from trials in the general population, there is a correlation between the level of neutralizing antibody to SARS-CoV-2 spike protein and symptomatic disease.
- The threshold for protection against severe COVID-19 is significantly lower than that required to prevent viral infection (15).
- Determination of protective levels of antibody is confounded by the wide variety of antibody tests that are commercially available, with no direct means to compare results from the different tests.
- The protective components of Cellular (T cell and NK T cells) and humoral responses (IgG/IgM vs IgA) may not be linked in individual SOT recipients; it is possible to have an active acquired or innate immune response in the absence of antibody and vice versa (3,6, 9,10). However, the clinical consequence of this divergence is not known nor measurable.
- Even in the absence of “protective antibody titers,” there is likely some protection against more severe disease after vaccination (16-18).
- Clinical effectiveness studies in the setting of SOT are lacking.
- While the level of immunosuppression, specifically the use of antiproliferative agents, has been implicated as a factor in poor antibody response after vaccination, there is no reliable guide to immunosuppression management in anticipation of vaccine responses.
- Booster vaccines will likely become necessary after time, even for the general public to maintain immunity (19, 20). However, at this time, when booster vaccination should be administered is not clear. From the existing data/experience, there are no reliable recommendations for booster dosing in SOT recipients who have not generated an antibody response with the initial doses. Some SOT recipients will increase their antibody titers to SARS-CoV-2 after booster mRNA vaccination (21, 22); this includes people who developed a response to the standard series and those who were initially “non-responders.” However, there are still a number of issues that remain unknown after booster vaccination. Because the majority of the available data examine kidney recipients and the most recent report examines the boosted response in patients who are beyond the first post-transplant year (median 99 months), it is unclear how to extrapolate these initial reports to the general SOT population. Despite 3 doses of mRNA vaccine, there are still non responders (up to a third in Kamar) and the cellular responses and neutralizing antibody to booster doses have not yet been reported in the studies of booster dosing. Safety data, in particular rejection, in SOT recipients are minimally reported at this time. Therefore,
- It is suggested that recipients who are concerned about their ongoing Covid risks after full vaccination discuss with their transplant physicians re: continued level of precautionary behavior to mitigate disease transmission/acquisition, testing and any new information about booster vaccination. Information about viral variants, vaccine effectiveness and perceived/real risk is changing rapidly. The transplant recipient’s concerns need to be addressed.
- There has been at least 1 report of rejection temporally following booster vaccination; the actual risk of rejection with additional doses of vaccine is unknown, however.
- There are no data currently to support adjustment of immunosuppression in anticipation of booster vaccination.
- While booster doses are not currently recognized under the EUA in the United States; international regulations may vary. We encourage people to follow clinical evidence and the local regulatory guidance regarding vaccine use/availability.
Based on the above information, we strongly recommend the following until further data are available:
- All solid organ transplant recipients should be vaccinated against SARS-CoV-2, using locally approved vaccines.
- All eligible household and close contacts of SOT recipients should be vaccinated against SARS-CoV-2 to minimize risks to the recipient.
- Whenever possible, vaccination should occur prior to transplantation (ideally with completion of vaccine series a minimum of 2 weeks prior to transplant).
- We support the development of institutional policies regarding pre-transplant vaccination as we believe that this is in the best interest of the transplant candidate, optimizing their chances of being safely transplanted, especially at times of greater infection prevalence.
- Routine antibody testing following vaccination is not recommended by the FDA. Considerations include:
- Most commercially available tests do not examine neutralizing antibody to the spike protein receptor binding domain (RBD).
- Many commercially available tests are qualitative.
- The analytical cut-off values for antibody detection are not necessarily the same as clinically relevant values.
- There is no commonly agreed upon titer that has been defined as protective against SARS-CoV-2 infection.
- Cellular responses may occur in the absence of measurable antibody
- However, individual physicians and patients may decide that antibody testing is desirable following a discussion regarding the interpretation of the test results and the consequences/risks of acquiring COVID-19 infection. There are many additional issues relevant to the patient, such as local prevalence of SARS-CoV-2 and its variants, personal situations relating to immunosuppression and transplant infections and the vaccination level in the household.
- In order to clarify the potential benefit of booster vaccinations for transplant recipients with uncertain response to the SARS-CoV-2 vaccines, we recommend that booster dosing occur in the context of clinical research studies. Monitoring of long-term responses and adverse effects are important to clarify existing clinical uncertainties.
- It is strongly recommended that all health care providers be vaccinated against SARS-CoV-2 to foster a safer environment for our patients.
- While COVID-19 variants continue to circulate in the community and the extent of protection is still unknown in transplant recipients, it is recommended that SOT candidates and recipients continue to adhere to protective measures including masking in public spaces, social distancing, frequent hand washing, and avoiding indoor crowds. The “mixed messaging” of uncertainty of vaccine efficacy for certain populations is recognized and requires more counseling from the transplant providers.
- We recommend ongoing monitoring of the regulatory and health department websites to obtain up to date COVID-19 prevalence and vaccine updates.
- We STRONGLY urge funding agencies to invest in research evaluating vaccine immunogenicity, vaccine effectiveness, and strategies to enhance vaccine responses in vulnerable populations, including SOT candidates and recipients, who may fuel the perpetuation of the pandemic.
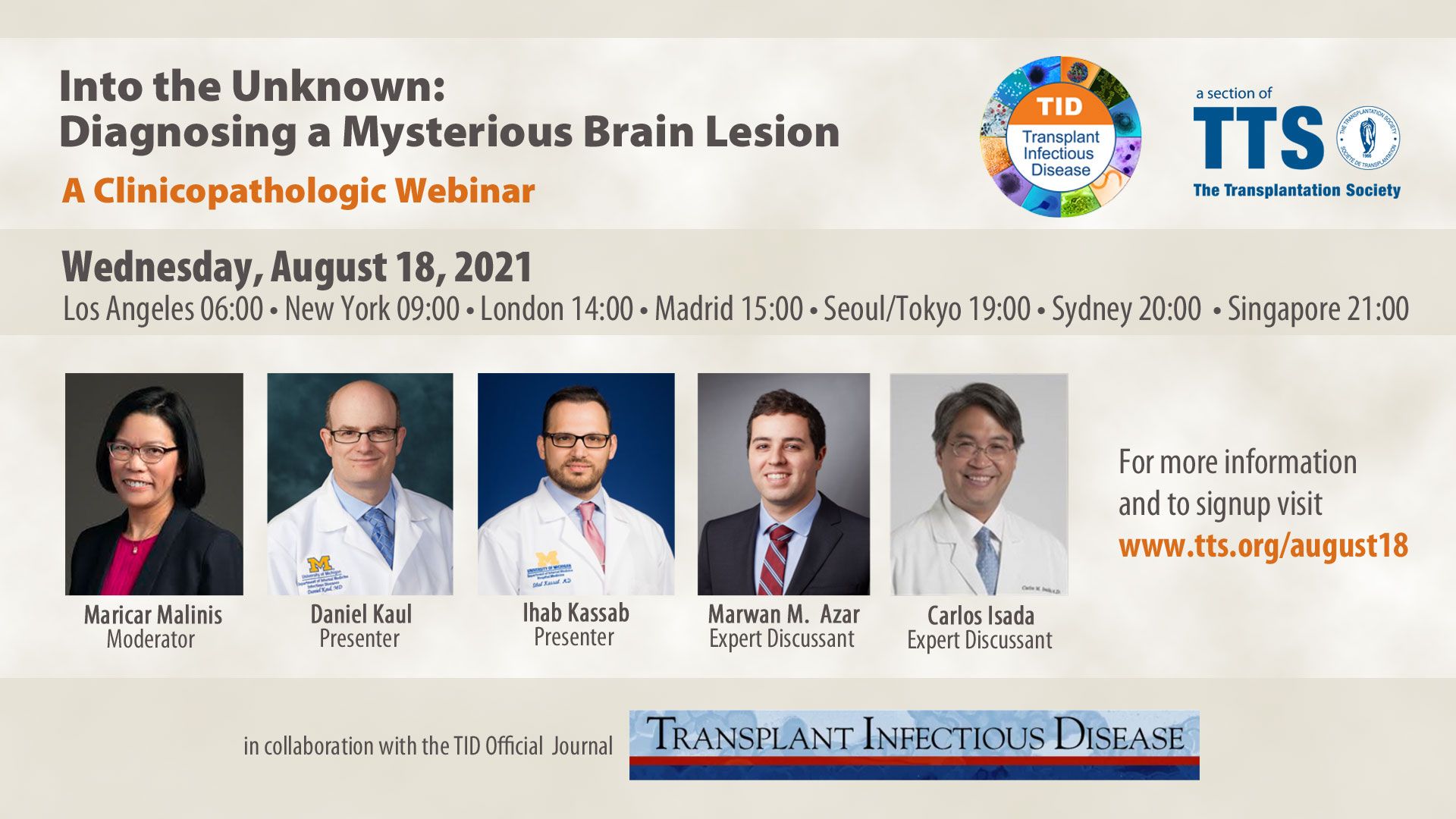
Upcoming August 18 TID-TTS Webinar
August 18, 2021
09:00 (-4 GMT - Montreal time)
Latest Videos Posted
Contact
Address
The Transplantation Society
International Headquarters
740 Notre-Dame Ouest
Suite 1245
Montréal, QC, H3C 3X6
Canada
Используйте Вавада казино для игры с бонусом — активируйте промокод и начните выигрывать уже сегодня!