Transplantation Direct - May 2018 - Volume 4 - Issue 5

This month in Transplantation Direct we feature a wide variety of topics in transplantation. For those interested in liver transplantation, performing transplants with a venovenous bypass is explored in a large single center Canadian study, and Duke surgeons present a case of complications associated with an accessory gallbladder. A Japanese group examines the safety of performing an adult living donor liver transplant in patients with portal vein thrombosis; other articles focus on the value of MRCP in diagnosing biliary anastomotic strictures, and on mechanisms involving endothelial cell dysfunction in the context of steatotic human livers. In heart transplantation, data supporting the feasibility of biomarker use for monitoring right heart pressures is introduced. For those interested in kidney transplantation, we have reports on modifiable factors associated with prolonged warm ischemia time, a modified Delphi Study in the UK related to optimizing listing for transplantation, and on the use of personalized patient evaluation protocols for making decisions on live donation. Lung transplant studies are also included in this issue, examining cyclophosphamide use for refractory acute cellular rejection, and an analysis of long-term outcomes in combined lung-liver transplants. We hope that you find this content useful and look forward to an article contribution from you soon.
TTS EDUCATION COMMITTEE WEBINAR SERIES
"TRENDS AND CHALLENGES IN LIVER TRANSPLANTATION"
TUESDAY, MAY 15, 2018 - 2:00 PM EDT (MONTREAL TIME)
KIDNEY PROBLEMS IN LIVER TRANSPLANTATION
 |
Moderator: Marcelo Cantarovich, MD Professor, Department of Medicine, Division of Nephrology, Faculty of Medicine, McGill University Montréal, QC, Canada |
 |
Discussant: Annmarie Huysman Liapakis, MD Assistant Professor of Medicine (Digestive Diseases), Yale School of Medicine New Haven, CT, USA |
 |
Discussant: Clifford D. Miles, MD, MS, FAST Associate Professor of Internal Medicine University of Nebraska Medical Center Omaha, NE, USA |
Survey study for transplant surgeons
Dr. Nancy Ascher and Dr. Chris Freise from the University of California, San Francisco, invite you to participate in a short survey study (5 minutes) on kidney transplantation in women with breast cancer. A diagnosis of breast cancer in a patient awaiting kidney transplantation might affect candidacy for receiving a transplant. Understanding how transplant surgeons make decisions in these situations could improve management recommendations and inform future trials. All participants will have the option of receiving the survey results. We appreciate your time!
Sindh Institute Of Urology And Transplant's Biomedical Ethics Centre Joins WHO Regional Activities

April 26 - The Centre of Biomedical Ethics and Culture (CBEC) of the Sindh Institute of Urology and Transplant (SIUT) was designated as a World Health Organisation (WHO) Collaborating Centre in Bioethics at a special ceremony held at the SIUT.
CLICK TO READ THE FULL ARTICLE
Hospital first in UK to introduce pioneering liver transplant technology
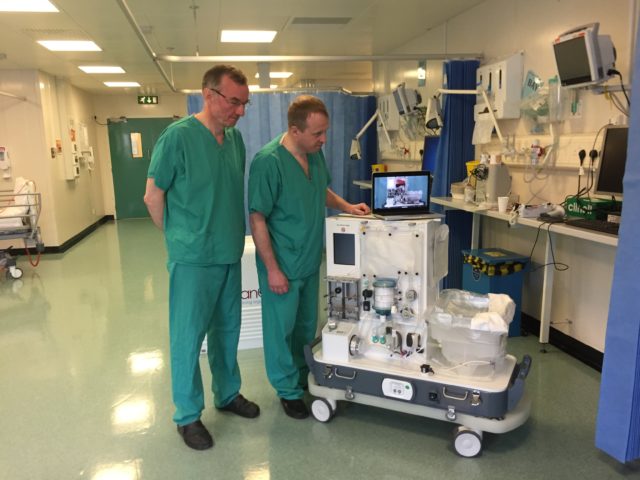
Professor Chris Watson and Andrew Butler with the new machine (Sally Wardle/PA).
May 2 - A hospital has become the first in the UK to bring state-of-the-art liver transplant technology into routine practice. Addenbrooke's Hospital in Cambridge will use machine perfusion, a process which can keep a liver "alive" outside the body for up to 24 hours by maintaining it at body temperature. The technology allows doctors to test how well a liver is functioning before transplant, boosting the chances the procedure will be a success. Addenbrooke's has become the only liver transplant centre in the UK to use the perfusion technique as part of its standard clinical practice.
In the News
Transflammation: A New Frontier In Regenerative Medicine
May 1 - Cardiovascular regeneration focuses on repairing or replacing damaged or senescent cardiac and vascular tissue. This damage is largely caused by myocardial ischemia (poor perfusion of the heart causing dysfunction or loss of cardiac tissue), fibrosis (with the replacement of myocytes and vessels with non-functional scar tissue) each of which may lead to heart failure, impaired functional capacity and quality of life, serious arrhythmias, and death.
CLICK TO READ THE FULL ARTICLE
Implantable islet cells come with their own oxygen supply
April 25 - Treating type-1 diabetes by transplanting islet cells becomes a trend but proven challenging. One impediment is that once the islets are transplanted, they will kick the bucket in the event that they don't get a sufficient supply of oxygen. Presently, scientists at MIT, working with an organization called Beta-O2 Technologies, have created and tried an implantable gadget that outfits islet cells with their own supply of oxygen, by means of a chamber that can be recharged like clockwork.
CLICK HERE TO READ THE ARTICLE
Organ Donation System Set For Changes
April 28 - NPR's Scott Simon speaks to transplant surgeon Dr. Dorry Segev about why the current system of organ allocation can be a death sentence for some patients.
THE HEART PRINTER
April 18 - THE IDEA:Bioprinting fully functioning human hearts to be used for transplants. Steven Morris, 53, started BioLife4D in 2016, bringing on board Jeffrey Morgan, the head of cardiothoracic transplantation at Baylor College of Medicine, as chief medical officer. Bioprinting a full-size human organ has never been done. But Morris and Morgan have devised a method they believe can work that involves extracting blood cells from a transplant candidate, reengineering them into heart cells, then 3D printing the heart cells layer by layer into a functioning organ—chambers, valves, and all.
Contact
Address
The Transplantation Society
International Headquarters
740 Notre-Dame Ouest
Suite 1245
Montréal, QC, H3C 3X6
Canada
Используйте Вавада казино для игры с бонусом — активируйте промокод и начните выигрывать уже сегодня!