SERVING THE INTERNATIONAL TRANSPLANTATION COMMUNITY

As we wish to bring our Congress to the entire international transplantation community, and in everyone’s individual time zone, we developed a program and schedule that would allow all delegates to access the Congress programming during two time periods regardless of geographic region.
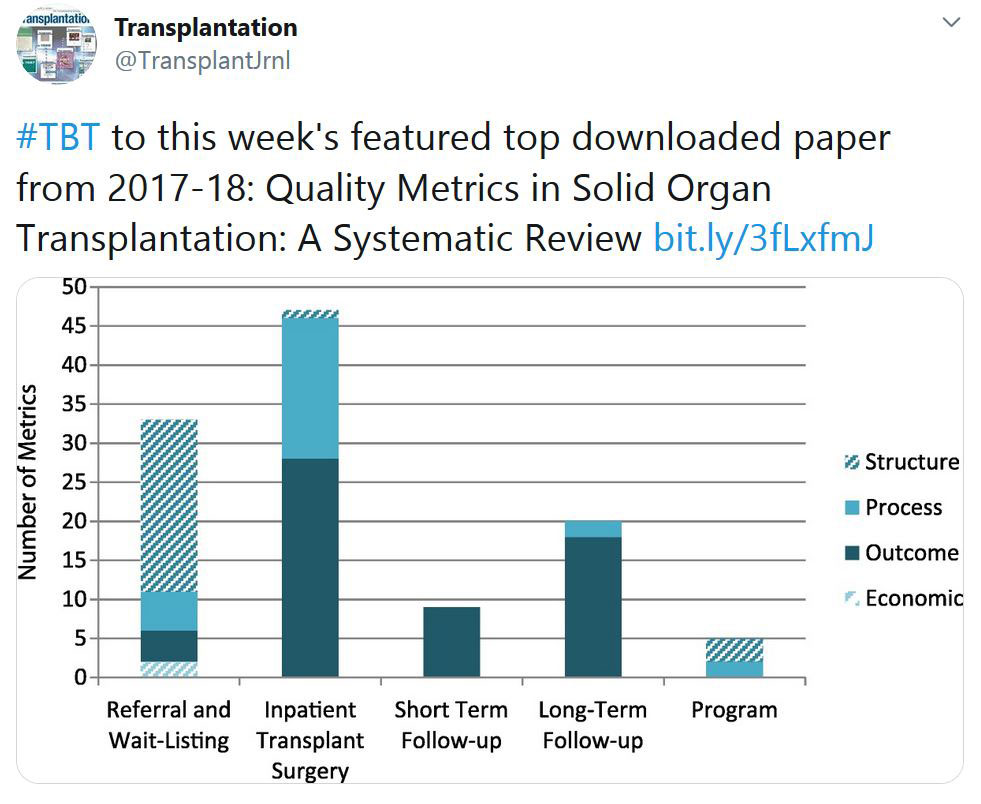
TRANSPLANTATION - WEEK'S MOST DOWNLOADED PAPER
CORONAVIRUS (COVID-19) UPDATE DASHBOARD
The Transplantation Society (TTS) and our journal Transplantation have developed online resources to keep you informed on the Coronavirus (COVID-19) outbreak.
- TTS Coronavirus (COVID-19) Dashboard
www.tts.org/covid-19 - Transplantation Global Transplantation COVID Report
www.tts.org/txjcovid19
We are also requesting contributions and news from the transplant community to be sent to covid-19@tts.org for inclusion on our resources page.
In this dashboard, you will find links to TTS and other global and regional resources, as well as interactive maps, publications and webinars. We encourage you to explore this dashboard and share with your colleagues.
Website - www.tts.org/covid-19
Editors and contributors to Transplantation have shared their thoughts on how they are dealing with the current crisis. While we understand that the information of today may be quite different tomorrow in this fast-moving pandemic, this report will open our forum of an international exchange on COVID for the transplant community.
Website - www.tts.org/txjcovid19
Please send your own contributions and news to covid-19@tts.org for inclusion on our resources page.
«HOT OFF THE PRESS» RECENT PUBLICATIONS IDENTIFIED BY TTS EDUCATION COMMITTEE ON COVID-19
This week's selection made by: Enver Akalin

COVIDSurg Collaborative*
LANCET May 29, 2020 https://doi.org/10.1016/S0140-6736(20)31182-X
This is an international, multicentre, cohort study at 235 hospitals in 24 countries included all patients undergoing surgery who had SARS-CoV-2 infection confirmed within 7 days before or 30 days after surgery. This article analyzes 1128 patients who had surgery between Jan 1 and March 31, 2020, of whom 835 (74·0%) had emergency surgery and 280 (24·8%) had elective surgery. SARS-CoV-2 infection was confirmed preoperatively in 294 (26·1%) patients. 30-day mortality was 23·8%. Pulmonary complications occurred in 51·2% of the patients; 30-day mortality in these patients was 38·0%. The authors reported risk factors for mortality.
Xavier Muller et al.
American Journal of Transplantation First published: 31 May 2020
https://doi.org/10.1111/ajt.16082
This article reports strategies and preliminary results in liver transplantation during the peak of the SARS‐CoV‐2 pandemic from a single‐center in France. The authors performed 10 successful liver transplantations during the peak of the pandemic with a short median intensive care unit stay (2,5 days), benchmark post‐transplant morbidity and no occurrence of SARS‐CoV‐2 infection during follow‐up.
Matthew J Cummings, Matthew R Baldwin, Darryl Abrams, Samuel D Jacobson, Benjamin J Meyer, Elizabeth M Balough, Justin G Aaron,
Jan Claassen, LeRoy E Rabbani, Jonathan Hastie, Beth R Hochman, John Salazar-Schicchi, Natalie H Yip, Daniel Brodie, Max R O’Donnell
LANCET May 19, 2020
https://doi.org/10.1016/S0140-6736(20)31189-2
This article reviewed 1150 adults who were admitted to between March 2 and April 1, 2020, with laboratory-confirmed COVID-19, of which 257 (22%) were critically ill. As of April 28, 2020, 39% patients had died, 79% patients received invasive mechanical ventilation, 31% received renal replacement therapy. Older age, chronic heart and lung disease, high IL6 and D-dimer levels were associated with mortality.
Anakinra for severe forms of COVID-19: a cohort study.
Thomas Huet, Hélène Beaussier, Olivier Voisin, Stéphane Jouveshomme, Gaëlle Dauriat, Isabelle Lazareth, Emmanuelle Sacco, Jean-Marc Naccache, Yvonnick Bézie, Sophie Laplanche, Alice Le Berre, Jérôme Le Pavec, Sergio Salmeron, Joseph Emmerich, Jean-Jacques Mourad, Gilles Chatellier, Gilles Hayem
Lancet Rheumatol 2020 Published Online May 29, 2020
https://doi.org/10.1016/S2665-9913(20)30164-8
This article reports 52 consecutive patients in the anakinra group and 44 historical patients who were identified in the Groupe Hospitalier Paris Saint-Joseph COVID cohort study from March 24 to April 6, 2020. Admission to the ICU for invasive mechanical ventilation or death occurred in 13 (25%) patients in the anakinra group and 32 (73%) patients in the historical group (hazard ratio [HR] 0・22 [95% CI 0・11–0・41; p<0・0001). The treatment effect of anakinra remained significant in the multivariate analysis (HR 0・22 [95% CI 0・10–0・49]; p=0・0002).
Antibody responses to SARS-CoV-2 in patients with COVID-19.
Quan-Xin Long et al.
Nature Medicine
https://doi.org/10.1038/s41591-020-0897-1
This article reports acute antibody responses to SARS-CoV-2 in 285 patients with COVID-19. Within 19 days after symptom onset, 100% of patients tested positive for antiviral immunoglobulin-G (IgG). Seroconversion for IgG and IgM occurred simultaneously or sequentially. Both IgG and IgM titers plateaued within 6 days after seroconversion. Serological testing may be helpful for the diagnosis of suspected patients with negative RT–PCR results and for the identification of asymptomatic infections.
IN THE NEWS
IN A MOLECULE, RESEARCHERS SEE POTENTIAL TO HELP ORGAN TRANSPLANTS THRIVE

May 28 - Scientists have made great strides in increasing success rates for organ transplants—at least through the first year after surgery. But a lingering long-term response of the recipient's immune system tends to erode the grafted tissue's health, and can eventually lead to organ failure.
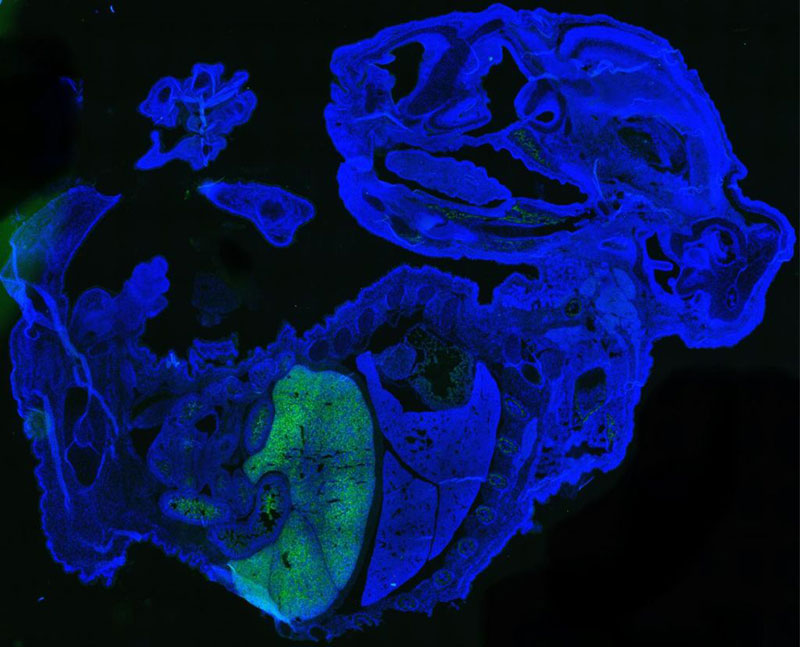
NEW HUMAN-MOUSE CHIMERA IS THE MOST HUMAN YET
May 29 - A newly-created mouse-human embryo contains up to 4% human cells — the most human cells yet of any chimera, or an organism made of two different sets of DNA.
THE FUTURE OF DIABETES: IMPROVING ISLET TRANSPLANTATION

May 27 - This year, the U.S. Food and Drug Administration is expected to approve islet transplants as a treatment for people with type 1 diabetes. The transplants, which deliver insulin-making cells to replace those lost to the disease, have been classified as experimental in the United States since they were first performed more than 20 years ago.
INEQUITIES IN ACCESS TO KIDNEY TRANSPLANTATION EXIST EVEN WITH UNIVERSAL HEALTHCARE
May 28 - A new study has uncovered inequities in access to kidney transplantation in the UK despite its universal healthcare system. The findings appear in an upcoming issue of CJASN.
BEYOND COLD STORAGE: TECHNOLOGY DESIGNED TO KEEP ORGANS WARM, HELPS LIVER TRANSPLANT PATIENTS IN KEY STUDY
May 26 - Since the 1960s, cold storage emerged as the preferred method for organ preservation for transplantation, but it didn’t tick all the boxes — limitations such as the risk of early graft dysfunction still contribute to chronic complications. So an upgrade was in order. Instead of flushing and preserving the procured organ at roughly freezing temperatures, new technology actually keeps the organs warm and toasty for transplantation in a bid to improve organ accessibility and improve transplantation outcomes.
UPCOMING MEETINGS AND ANNOUNCEMENTS
11th International Pediatric Intestinal Failure and Rehabilitation Symposium
International Transplantation Science Meeting
ITS 2021 meeting in the San Diego area — October 17-20, 2021
After careful consideration, and in light of the ongoing Coronavirus developments, we’ve made the difficult decision to postpone the ITS 2020 Meeting in Europe to 2022. Stay tuned for dates and location.
We would like to take this opportunity to confirm that we will have the 2021 ITS meeting in the San Diego area from October 17-20, 2021.
Further details will be available this summer.
We look forward to hosting you in California next year.
Until then, stay safe and healthy!
Contact
Address
The Transplantation Society
International Headquarters
740 Notre-Dame Ouest
Suite 1245
Montréal, QC, H3C 3X6
Canada
Используйте Вавада казино для игры с бонусом — активируйте промокод и начните выигрывать уже сегодня!