TTS 2020 Virtual Congress - Extended Registration Deadline
TTS 2020 VIRTUAL CONGRESS
CALL FOR VIRTUAL NETWORKING LOUNGE IDEAS
Half the reason people attend congresses is to network.
Submission Deadline - August 14, 2020
Sessions will range from 45 to 90 minutes in length with multiple time zones to choose from. All sessions will be hosted on the Zoom platform managed by the technology team at TTS. The maximum capacity for each session is 300, however we recommend keeping groups much smaller (10 to 50 participants) to ensure interactivity. Our scientific program committee will work with respondents (when needed) to refine their proposals as well as assist in finding experts (when necessary).

JUST RELEASED - TRANSPLANTATION DIRECT - AUGUST ISSUE
The August issue of Transplantation Direct covers a wide-variety of topics in transplantation. Among the areas covered includes an interesting exchange of letters presented on an article we recently published regarding the Fiqh Council of North America's 2018 ruling on organ donation and transplantation. As a review article, we have a timely overview on COVID-19 in kidney transplantation related to epidemiology, patient management and impact. There are three experimental studies on strategies to reduce ischemia reperfusion injury, including use of NRF2 activators in liver (rat), normothermic ex vivo perfusion (pig) or free radical scavengers (PrC-210) in (rat) kidney grafts. Diagnostic-oriented studies are presented on: (1) the use of DNA demethylation assays to estimate immune system "age", (2) donor-derived cell-free DNA + Banff assessments to predict long-term kidney function, (3) MRI use for the non-invasive diagnosis of interstitial kidney fibrosis, (4) Doppler ultrasound of kidney transplants to determine cardiovascular risk factors, and (5) urinary cell transcriptome analysis to predict simultaneous cellular and antibody-mediated rejection in kidney transplantation. In other areas of transplantation research, we have an experimental article on preclinical allogeneic nerve transplantation, and a survey-based study on developing a tool-set for maximizing proper patient access to organ transplantation programs. With momentum for bringing xenotransplantation to the clinic, we have an article that proposes model options for preclinical testing. Also, for our bone marrow transplant readership, scientists report on the use of purified CD34+CD90+CD45RA- cells in a non-human primate model for allogeneic hematopoietic stem cell transplantation. Please find all the details in open access on our Transplantation Direct website.
TRANSPLANTATION DIRECT - HIGHLIGHTED ARTICLE
Dr. Jeremy R. Chapman, Editor-in-Chief, Transplantation
Early Experiences With COVID-19 Testing in Transplantation
Boyarsky BJ, Massie AB, Love AD, et al.
Transplantation Direct: July 2020 - Volume 6 - Issue 7 - p e572
In these times where we are all threatened in a variety of ways by the pandemic of COVID-19 flowing almost unhindered around the world. We have all been craving information on the direct impact on our programs, our staff, our patients and our donors. In this paper the Johns Hopkins Health System have put together their perspectives on these issues. The paper confirms what the TTS COVID-19 website also provides: Healthcare workers and donors have very low rates of infection at 0-1, though of course even a single infected healthcare worker can have a major impact on a transplant program. Patients with end stage kidney disease and with transplants had infection rates of 17-20%. Mortality has been reported as very high by many places – such as in Paris, London and New York - and the Baltimore experience reflects that too. COVID is a story that will run and run – as they say – but many of the important answers which influence how we work are already known.
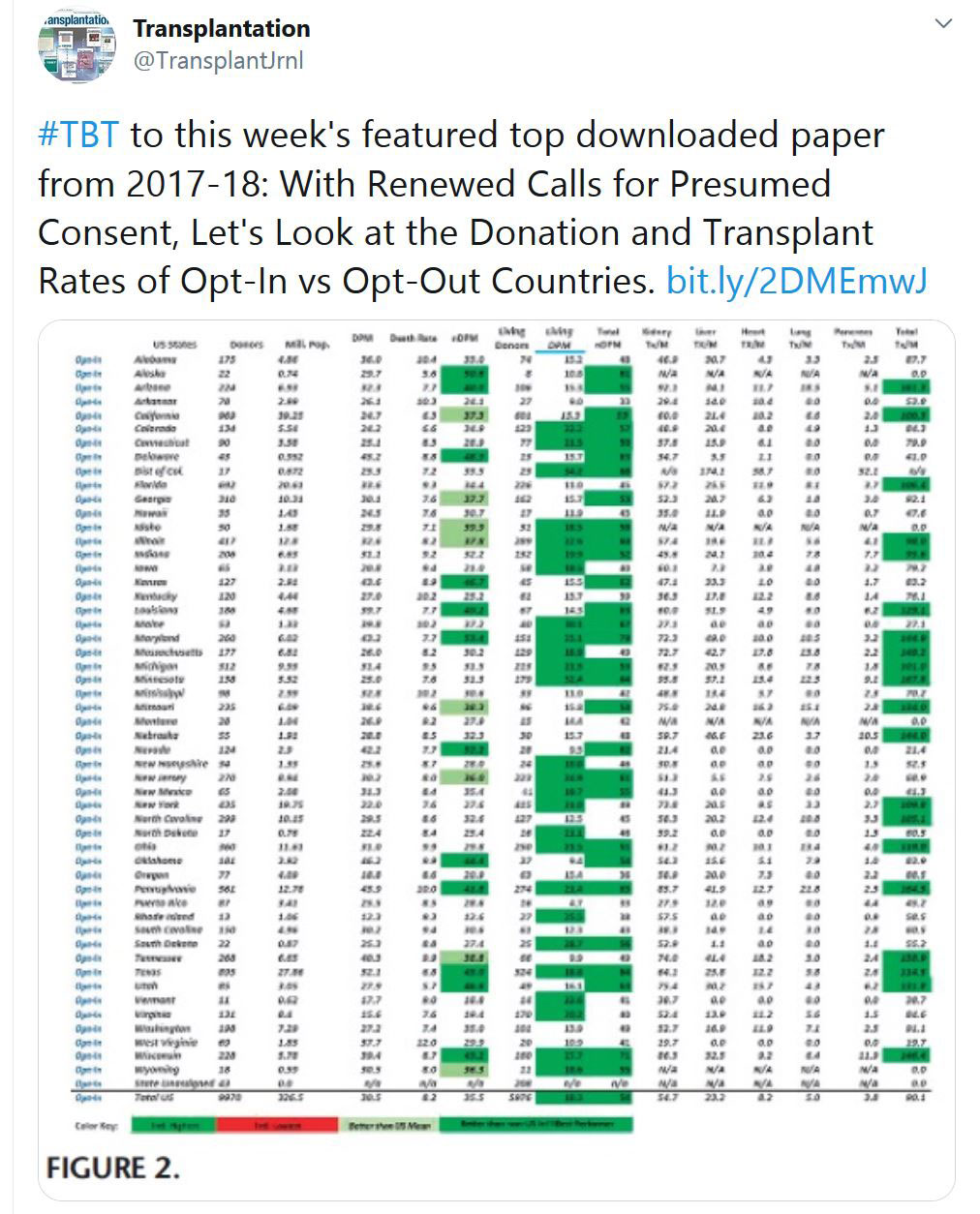
TRANSPLANTATION - WEEK'S MOST DOWNLOADED PAPER
«HOT OFF THE PRESS»
RECENT PUBLICATIONS IDENTIFIED BY TTS EDUCATION COMMITTEE ON COVID-19
COVID-19 in solid organ transplant: A multi-center cohort study
Olivia Kates et al. UW COVID-19 SOT Study Team
Clin Infect Dis 2020 Aug 7;ciaa1097. doi: 10.1093/cid/ciaa1097.
Four hundred eighty-two SOT recipients from >50 transplant centers were included: 318 (66%) kidney or kidney/pancreas, 73 (15.1%) liver, 57 (11.8%) heart, and 30 (6.2%) lung. Median age was 58 (IQR 46-57), median time post-transplant was 5 years (IQR 2-10), 61% were male, and 92% had ≥1 underlying comorbidity. Among those hospitalized (376 [78%]), 117 (31%) required mechanical ventilation, and 77 (20.5%) died by 28 days after diagnosis. Specific underlying comorbidities (age >65 [aOR 3.0, 95%CI 1.7-5.5, p<0.001], congestive heart failure [aOR 3.2, 95%CI 1.4-7.0, p=0.004], chronic lung disease [aOR 2.5, 95%CI 1.2-5.2, p=0.018], obesity [aOR 1.9, 95% CI 1.0-3.4, p=0.039]) and presenting findings (lymphopenia [aOR 1.9, 95%CI 1.1-3.5, p=0.033], abnormal chest imaging [aOR 2.9, 95%CI 1.1-7.5, p=0.027]) were independently associated with mortality. Multiple measures of immunosuppression intensity were not associated with mortality.
COVID‐19 in lung transplant recipients: A single center case series from New York City
Meghan Aversa, Luke Benvenuto, Michaela Anderson, Lori Shah, Hilary Robbins, Marcus Pereira, Jenna Scheffert, Maggie Carroll, Jamie Hum, Margaret Nolan, Genevieve Reilly, Philippe Lemaitre, B. Payne Stanifer. Frank D’Ovidio, Joshua Sonett, Selim Arcasoy
American Journal of Transplantation, published 09 August 2020 https://doi.org/10.1111/ajt.16241
This article describes 32 lung transplant patients who developed mild (16%), moderate (44%), or severe (41%) COVID‐19. 11 patients (34%) died at a median time of 14 days from admission. Complications during admission included: acute kidney injury (63%), transaminitis (31%), shock (31%), acute respiratory distress syndrome (25%), neurological events (25%), arrhythmias (22%), and venous thromboembolism (9%). Compared to patients with moderate COVID‐19, patients with severe COVID‐19 had higher peak white blood cell counts (15.8 vs. 7 x 103/uL, p=0.019), C‐reactive protein (198 vs. 107 mg/L, p=0.010) and D‐dimer (8.6 vs. 2.1 ug/mL, p=0.004) levels, and lower nadir lymphocyte counts (0.09 vs. 0.4x 103/uL, p=0.006). COVID‐19 is associated with severe illness and a high mortality rate in lung transplant recipients.
SARS-CoV-2 viral load predicts COVID-19 mortality
Elisabet Pujadas, Fayzan Chaudhry, Russell McBride, Felix Richter, Shan Zhao, Ania Wajnberg, Girish Nadkarni, Benjamin S Glicksberg, Jane Houldsworth, Carlos Cordon-Cardo
Lancet Respir Med 2020 Published Online August 6, 2020 https://doi.org/10.1016/ S2213-2600(20)30354-4
Viral loads for symptomatic, hospitalized 1145 patients who tested positive for SARS-CoV-2 were measured on samples collected between March 13 and May 4, 2020. A Cox proportional hazards model adjusting for age, sex, asthma, atrial fibrillation, coronary artery disease, chronic kidney disease, chronic obstructive pulmonary disease, diabetes, heart failure, hypertension, stroke, and race yielded a significant independent association between viral load and mortality (hazard ratio 1·07 [95% CI 1·03–1·11], p=0·0014), with a 7% increase in hazard for each log transformed copy per mL. A univariate survival analysis revealed a significant difference in survival probability between those with high viral load (defined as being greater than the overall mean log10 viral load of 5·6 copies per mL) and those with low viral load (p=0·0003), with a mean follow-up of 13 days (SD 11) and a maximum follow-up of 67 days.
Systems-level immunomonitoring from acute to recovery phase of severe COVID-19
Lucie Rodriguez, Pirkka T. Pekkarinen, Tadepally Lakshmikanth, Ziyang Tan, Camila Rosat Consiglio, Christian Pou, Yang Chen, Constantin Habimana Mugabo, Ngoc Anh Nguyen, Kirsten Nowlan Tomas Strandin, Lev Levanov, Jaromir Mikes, Jun Wang, Anu Kantele, Jussi Hepojoki, Olli Vapalahti, Santtu Heinonen, Eliisa Kekäläinen, Petter Brodi
Cell Reports Medicine (2020) doi: https://doi.org/10.1016/j.xcrm.2020.100078
This article reports on a systems-level blood immunomonitoring study of 37 adult patients diagnosed with COVID-19 and followed with up to 14 blood samples from acute to recovery phases of the disease. The authors describe an IFNγ – Eosinophil axis activated prior to lung hyperinflammation and changes in cell-cell coregulation during different stages of the disease. The study also maps an immune trajectory during recovery that is shared among patients with severe COVID-19.
CORONAVIRUS (COVID-19) UPDATES
The Transplantation Society (TTS) and our journal Transplantation have developed online resources to keep you informed on the Coronavirus (COVID-19) outbreak.
- TTS Coronavirus (COVID-19) Dashboard
www.tts.org/covid-19 - Transplantation Global Transplantation COVID Report
www.tts.org/txjcovid19
We are also requesting contributions and news from the transplant community to be sent to covid-19@tts.org for inclusion on our resources page.
In this dashboard, you will find links to TTS and other global and regional resources, as well as interactive maps, publications and webinars. We encourage you to explore this dashboard and share with your colleagues.
Editors and contributors to Transplantation have shared their thoughts on how they are dealing with the current crisis. While we understand that the information of today may be quite different tomorrow in this fast-moving pandemic, this report will open our forum of an international exchange on COVID for the transplant community.
Website - www.tts.org/txjcovid19
Please send your own contributions and news to covid-19@tts.org for inclusion on our resources page.
IN THE NEWS
DAMAGED HUMAN LUNGS SUCCESSFULLY RECOVERED
Aug. 4 - For the first known time, a severely injured human lung that failed to recover using standard clinical EVLP was successfully recovered during a twenty-four hour period on the multidisciplinary team’s cross circulation platform, a report of the process was published in Nature Medicine.
MOVE OVER AKITA: INTRODUCING ‘KUMA MUTANT’ MICE FOR ISLET TRANSPLANTATION RESEARCH
Aug. 5 - Scientists at the Tokyo Institute of Technology (Tokyo Tech) have used a gene editing technique to establish a novel mouse model of permanent neonatal diabetes—the immune-deficient Kuma mutant mice with a specific deletion in the Insulin2 (Ins2) gene.
FOR THE FIRST TIME, A WOMAN IN THE U.S. GETS A SECOND FACE TRANSPLANT

Aug. 7 - For the second time in a decade, a New Hampshire woman has a new face. Carmen Blandin Tarleton, whose face was disfigured in an attack by her ex-husband, became the first American and only the second person globally to undergo the procedure after her first transplant began to fail six years after the operation. The transplant from an anonymous donor took place at Boston's Brigham and Women’s Hospital in July.
THE ORGAN TRANSPLANT AFTERSHOCK
Aug. 5 - A listener asks a question about organ donations in the time of covid-19 … and her question leads Martine down a rabbit hole on the current state of organ transplantation in the United States.
OUTCOMES FOLLOWING LISTING POLICY CHANGE FOR SIMULTANEOUS LIVER-KIDNEY TRANSPLANTATION

Aug. 6 - The listing policy for simultaneous liver-kidney transplantation issued on July 10, 2017, imposed more stringent criteria on recipient renal function. Data on recipient outcomes following the change are scarce. M. L. Samoylova and colleagues at Duke University Hospital, Durham, North Carolina, conducted an analysis to examine outcomes prior to and following the policy change.
Q AND A: HOW A RESEARCHER IS USING TECHNOLOGY TO GROW THE WORLD’S FIRST NOVEL HUMAN ORGAN
Aug. 6 - Ian Bolland, editor of MPN’s sister title Med-Tech Innovation, spoke to Dr Sam Pashneh-Tala, a research fellow at the University of Sheffield. Dr Pashneh-Tala is researching the fabrication of blood vessels in unique geometries for use in surgery, developing new medical devices, or studying conditions like cardiovascular disease. Dr. Pashneh-Tala has used Formlabs printers to design and create the blood vessel mould from the custom Biodegradable Polymer Emulsion he and his team developed.
UPCOMING MEETINGS AND ANNOUNCEMENTS
TTS BUSINESS MEETING

In accordance with the TTS By-Laws, a Business Meeting will be held shortly after the close of the TTS 2020 Virtual Congress. The meeting will be help on Sunday, September 20, at 8 AM Montreal time and will last approximately one hour. The agenda will include an update on the TTS finances, the announcement of the TTS 2024 Congress location, a presentation for the TTS 2022 Congress in Buenos Aires, the announcement of the 2020-2022 Councilors and Officers and the official change of TTS Presidency. All members are invited to participate.
As this meeting will be virtually, we will send all members a link to join this meeting shortly before the meeting takes place.
Sincerely,
John Fung
Secretary, The Transplantation Society
18th Asian Pacific Congress of Nephrology (APCN)
IPITA-IXA-CTRMS Joint Congress
Contact
Address
The Transplantation Society
International Headquarters
740 Notre-Dame Ouest
Suite 1245
Montréal, QC, H3C 3X6
Canada
Используйте Вавада казино для игры с бонусом — активируйте промокод и начните выигрывать уже сегодня!