TRANSPLANTATION - HIGHLIGHTED ARTICLE
Dr. Jeremy R. Chapman, Editor-in-Chief, Transplantation
Natural Killer Cells: Critical Effectors During Antibody-Mediated Rejection of Solid Organ Allografts
Miyairi S, Baldwin WM, Valujskikh A, et al.
Transplantation: May 5, 2020 - Volume Online First
Antibody mediated rejection (AMR) remains a conundrum for all of the organ transplant programs – while we might believe we understand T Cell mediated rejection, only the optimist has the same settled view of AMR. In this great review, these authors dissect the role of Natural Killer Cells as part of the interaction of donor specific antibodies with the innate immune system as critical to AMR in both experimental models and clinical practice. The lead that this data provides to new targets for immune suppression should give us a chance to further improved results.
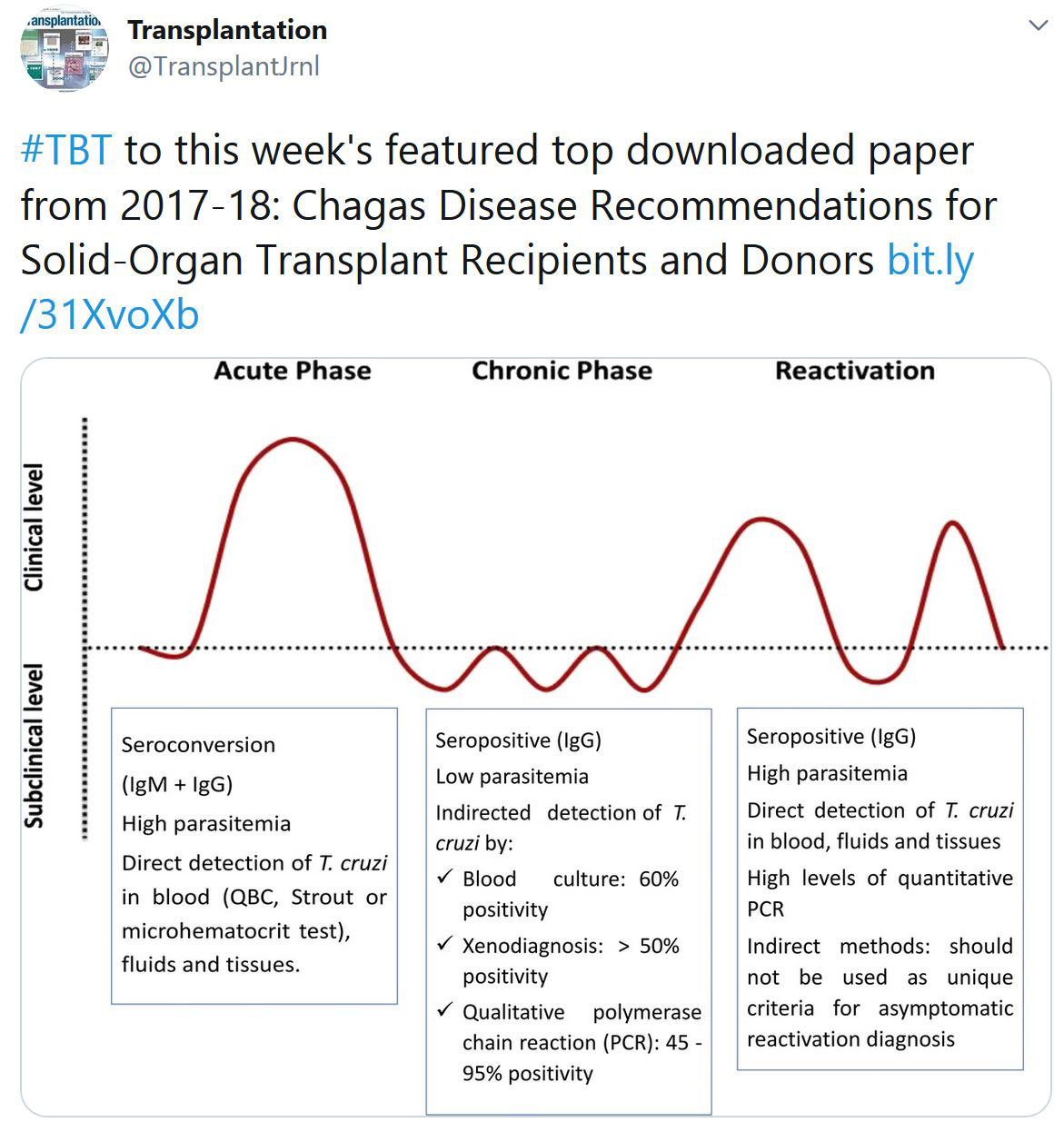
TRANSPLANTATION - WEEK'S MOST DOWNLOADED PAPER
ISN-TTS Webinar: Donor/Recipient pair - Risks vs. Gains - Cancer
Women in Transplantation Virtual Event – October 30, 2020
Women in Transplantation is proud to partner with FOCIS on this very important and relevant session Diversity, Sex and Gender in the COVID Era presented by Stanford's Senior Associate Dean for Faculty Development and Diversity, Yvonne Maldonado, MD.
In this presentation, Dr. Maldonado will reflect upon her own career journey and discuss research on gender, its intersection with other marginalized social identities, and its role in the academic workplace. She will expand upon her research as an infectious disease epidemiologist as well as research and personal experiences during today’s COVID-19 era.
The session will be moderated by Dr. Megan Sykes, Michael J. Friedlander Professor of Medicine and Professor of Microbiology & Immunology and Surgical Sciences (in Surgery) and Director, Columbia Center for Translational Immunology, ex WIT Co-Chair and President-Elect of FOCIS.
Join us on Friday October 30th at 11:15am by registering at this link below:
Click here to register for the event
FREE REGISTRATION for WIT & TTS Members!
Registration details will be sent on to all registered closer to the time.
«HOT OFF THE PRESS»
RECENT PUBLICATIONS IDENTIFIED BY TTS EDUCATION COMMITTEE ON COVID-19
COVID-19 infection in kidney transplant recipients at the epicenter of pandemics
Yorg Azzi et al.
Kidney International. (October 2020), doi: https://doi.org/10.1016/j.kint.2020.10.004.
This article investigated the prevalence and clinical outcomes of COVID-19 in recipients of kidney transplants in the Bronx, New York. Between March 16 and June 2, 2020, 132 kidney transplant recipients tested positive by SARS-CoV-2 RT-PCR. From May 3 to July 29, 2020, 912 kidney transplant recipients were screened for SARS-CoV-2 IgG antibodies during routine clinic visits, of which 16.6% tested positive. Fifty-five of the 152 patients had previously tested positive by RT-PCR, while the remaining 97 did not have significant symptoms and had not been previously tested by RT-PCR. The prevalence of SARS-CoV-2 infection was 23.4% in the 975 patients tested by either RT-PCR or SARS-CoV-2 IgG. Older patients and patients with higher serum creatinine levels were more likely diagnosed by RT-PCR compared to SARS-CoV-2 IgG. Sixty-nine RT-PCR positive patients were screened for SARS-CoV-2 IgG antibodies at a median of 44 days post-diagnosis (Inter Quartile Range 31-58) and 80% were positive. Overall mortality was 20.5% but significantly higher (37.8%) in the patients who required hospitalization. 23% of the hospitalized patients required kidney replacement therapy and 6.3% lost their allografts. In multivariable analysis, older age, receipt of deceased-donor transplantation, lack of influenza vaccination in the previous year and higher serum interleukine-6 levels were associated with mortality. Thus, 42% of patients with a kidney transplant and with COVID-19 were diagnosed on antibody testing without significant clinical symptoms, 80% of patients with positive RT-PCR developed SARS-CoV-2 IgG and mortality was high among patients requiring hospitalization.
Results from the ERA-EDTA Registry indicate a high mortality due to COVID-19 in dialysis patients and kidney transplant recipients across Europe
Kitty Jager et al.
Kidney International. (October 2020) PMID: 32979369. DOI: 10.1016/j.kint.2020.09.006
This article investigated 28-day mortality after COVID-19 diagnosis in the European kidney replacement therapy population. Data on all patients with a diagnosis of COVID-19 were collected from seven European countries encompassing 4298 patients. COVID-19 attributable mortality was calculated using propensity-score matched historic controls and after 28 days of follow-up was 20.0% (95% confidence interval 18.7%-21.4%) in 3285 patients receiving dialysis, and 19.9% (17.5%-22.5%) in 1013 recipients of a transplant. The authors identified differences in COVID-19 mortality across countries, and an increased mortality risk in older patients receiving kidney replacement therapy and male patients receiving dialysis. In recipients of kidney transplants older than 75 years of age 44.3% (35.7%-53.9%) did not survive COVID-19. Mortality risk was 1.28 (1.02-1.60) times higher in transplant recipients compared with matched dialysis patients. Thus, the pandemic has had a substantial effect on mortality in patients receiving kidney replacement therapy; a highly vulnerable population due to underlying chronic kidney disease and high prevalence of multimorbidity.
COVID‐19 Outcomes in Patients Waitlisted for Kidney Transplantation and Kidney Transplant Recipients
Rebecca Craig‐Schapiro et al.
American Journal of Transplantation.12 October 2020 https://doi.org/10.1111/ajt.16351
This article studied 56 waitlisted patients and 80 kidney transplant recipients diagnosed with COVID‐19 between March 13‐ May 20, 2020. Despite similar demographics and burden of comorbidities between waitlisted and transplant patients, waitlisted patients were more likely to require hospitalization (82% vs. 65%, p=0.03) and were at a higher risk of mortality (34% vs. 16%, p=0.02). Intubation was required in one‐third of hospitalized patients in each group, nd portended a very poor prognosis. The vast majority of patients who died were male (84% waitlist, 100% transplant). Multivariate analysis demonstrated waitlist status, age, and male sex were independently associated with mortality. COVID‐19 has had a dramatic impact on waitlisted patients, decreasing their opportunities for transplantation and posing significant mortality risk.
CORONAVIRUS (COVID-19) UPDATES
INVITATION TO PARTICIPATE

Dear Members,
Researchers at McGill University are currently conducting a study entitled LIST-COVID-19 to study the impact of the COVID-19 pandemic on transplantation activity, volumes and immunosuppression practices on a global scale. The study will also help better understand the current and anticipated risks to transplantation during the pandemic and inform clinical practice during the “ramp-up” phase. The Transplantation Society is supporting the project, as well as several National and International Societies.
They are looking for physicians who take care of patients with a solid organ transplant to take a 10-15 minute survey on behalf of their center and program. Please note this is not a patient registry and no specific patient-level data is being collected. Please be assured they will only perform a collective analysis of the survey questions and no personal information identifying the participants will be divulged. The survey responses will be confidential. If you are interested in participating, please contact them at the emails listed below.
Investigators: Shaifali Sandal, MD and Marcelo Cantarovich, MD
Contact: shaifali.sandal@mcgill.ca and marcelo.cantarovich@muhc.mcgill.ca
The Transplantation Society (TTS) and our journal Transplantation have developed online resources to keep you informed on the Coronavirus (COVID-19) outbreak.
- TTS Coronavirus (COVID-19) Dashboard
www.tts.org/covid-19 - Transplantation Global Transplantation COVID Report
www.tts.org/txjcovid19
We are also requesting contributions and news from the transplant community to be sent to covid-19@tts.org for inclusion on our resources page.
In this dashboard, you will find links to TTS and other global and regional resources, as well as interactive maps, publications and webinars. We encourage you to explore this dashboard and share with your colleagues.
Editors and contributors to Transplantation have shared their thoughts on how they are dealing with the current crisis. While we understand that the information of today may be quite different tomorrow in this fast-moving pandemic, this report will open our forum of an international exchange on COVID for the transplant community.
Website - www.tts.org/txjcovid19
Please send your own contributions and news to covid-19@tts.org for inclusion on our resources page.

IN THE NEWS
ARTIFICIAL INTELLIGENCE MAY IMPROVE HEART TRANSPLANT OUTCOMES
Oct. 14 - NIH will fund a project exploring the ability of artificial intelligence to determine the likelihood of patients accepting or rejecting heart transplants.
MATERNAL FECAL MICROBIOTA TRANSPLANTATION IN C-SECTION BABIES CAN RESTORE THE GUT MICROBIOTA, SUGGESTS A PROOF-OF-CONCEPT STUDY

Oct. 16 - The microbiota of infants born by caesarean section resembles that of maternal oral cavity and skin, whereas that of vaginally born infants resembles that of the maternal gut microbiome. A new proof-of-concept study shows that the gut microbiota of C-section-born infants can be restored after delivery via orally administered maternal fecal microbiota transplantation.
OUTCOMES ASSOCIATED WITH PANCREAS TRANSPLANT IN PATIENTS WITH CKD AND TYPE 1 DIABETES

Oct. 14 - Both pancreas transplantation alone (PTA) and islet cell transplantation (ICT) have been associated with peri-operative declines in estimated glomerular filtration rate (eGFR), a decline that is less than that associated with medically managed diabetes. According to Rashikh Choudhury, MD, and colleagues in the department of surgery-division of transplantation surgery at the University of Colorado Hospital, Aurora, PTA and ICT have demonstrated long-term stabilization of chronic kidney disease (CKD) in patients with type 2 diabetes.
NICORD IMPROVES EFFICACY OF BONE MARROW TRANSPLANT FOR HEMATOLOGIC MALIGNANCIES
Oct. 13 - A phase 3 trial of omidubicel has shown the graft modality superior to standard umbilical cord blood for bone marrow transplantation in patients with hematologic malignancies, according to topline data released by the agent’s manufacturer.
UPCOMING MEETINGS AND ANNOUNCEMENTS
3rd IPITA/JDRF/HSCI Virtual Summit on Stem Cell Derived Beta Cells
The International Pancreas & Islet Transplant Association (IPITA) Conference Organizing Committee is committed to bringing the community together virtually.
International Transplantation Science Meeting (ITS 2021)

IPITA-IXA-CTRMS Joint Congress
FOCIS 2020 Virtual Annual Meeting
TTS members are invited to attend the FOCIS 2020 Virtual Annual Meeting – THE meeting in translational immunology!
The Federation of Clinical Immunology Societies exists to improve human health through immunology.
The FOCIS 2020 Virtual Annual Meeting on October 28-31, 2020, brings together an interdisciplinary group of world-renowned physicians and researchers to share the latest findings on diseases impacting the immune system.
Asian Transplantation Week (ATW) 2020
Contact
Address
The Transplantation Society
International Headquarters
740 Notre-Dame Ouest
Suite 1245
Montréal, QC, H3C 3X6
Canada
Используйте Вавада казино для игры с бонусом — активируйте промокод и начните выигрывать уже сегодня!