In Memoriam - Sir Peter Morris (1934-2022)
We are sad to announce the passing of TTS Medawar Laureate Sir Peter Morris
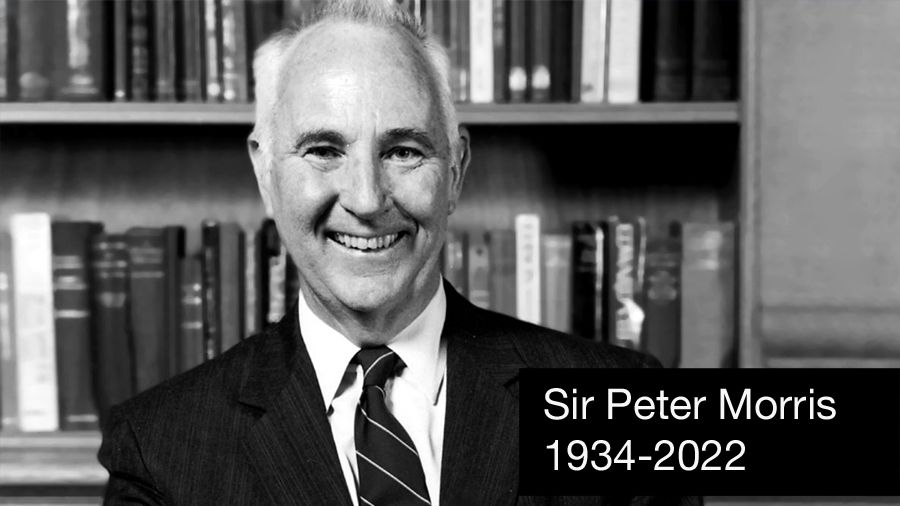
Sir Peter John Morris, Emeritus Nuffield Professor of Surgery University of Oxford an innovative surgeon scientist, dynamic leader and devoted educator.
Peter Morris was born in Horsham, in the state of Victoria, Australia. He studied engineering at Melbourne University, before switching to study Medicine. He graduated in 1957 and married Jocelyn (Joce), also a doctor, 3 years later. While Peter was a young Surgical Registrar at St Vincent’s’ Hospital in Melbourne, Dr Claude Welch from the Massachusetts General Hospital (MGH) came to St Vincent's as a Visiting Professor, this would prove to be important for his future surgical career. In order to gain additional clinical experience Peter and Joce came to work in the UK working their passage as a ships doctor on a cargo ship. Peter was as a surgical trainee at the Hammersmith Hospital in London before moving to Southampton as a registrar. Peter's interest in transplantation was probably initially triggered at the Hammersmith, as the first living unrelated kidney transplant was performed while he was there.
In 1964 Peter, Jocelyn and their first child moved to Boston. It was as a result of assisting Dr Welch during surgery while he was in Melbourne that Peter was appointed as a surgical resident at the MGH where he also began his research career working with Dr Jack Burke investigating defence mechanisms in models of surgical infection. Peter shared with confidents that he had never worked so hard as when he was a surgery resident at the MGH. It was during this time that Peter met Tony Monaco (TTS President 1986-1988) who was working in Dr Paul Russell's laboratory just across the corridor. Tony and his wife became life-long friends.
Peter and the family had originally planned to return to Melbourne, but the post he was to return to had been frozen due to a financial crisis at the university. Instead, David Hume invited him to set up a tissue-typing laboratory at the Medical College of Virginia to support the developing transplant programme. Here Peter became interested in the role of antibodies in transplantation. Together with Paul Terasaki, he discovered that donor specific cytotoxic antibodies did develop after transplantation and that if they were present at the time of transplantation, they could trigger hyperacute rejection of the transplanted organ.
At the end of 1967 Peter did return to Melbourne as a transplant and vascular surgeon and set up the tissue typing and immunology laboratories. Alan Ting joined Peter as his first graduate student to continue the study of the complex role antibodies play in transplantation.
Peter moved to Oxford with Joce and their five children in 1974 as Nuffield Professor of Surgery and Fellow of Balliol College. Several of Peter's colleagues from Melbourne moved to Oxford with him including John Fabre, Peter's second graduate student in Melbourne, and Alan Ting. Together they established a tissue typing laboratory and immunology research programme alongside the clinical transplant service. Sir Peter Medawar opened the first dedicated transplant unit at the Churchill Hospital in Oxford in 1978. The Oxford clinical and research programmes grew and soon attracted excellent clinical fellows and post-doctoral scientists as well as training numerous surgeon and physician scientists and immunologists, many of whom now run clinical and research programmes around the world. Peter, together with his Oxford colleagues, was a prolific author publishing widely in the scientific and surgical literature. His book, Kidney Transplantation is in its 8th edition, and he was the founding editor of the Oxford Textbook of Surgery.
Peter was a life-long supporter of The Transplantation Society. He organised the Brighton Congress in 1982, was elected as TTS President 1984-1986 and awarded the Medawar Prize in 2006. Peter served as an Editor of Transplantation from 1976 to 2014.
Peter was an accomplished sportsman representing Melbourne University at cricket, Australia at baseball and rather bizarrely, France at golf. The annual cricket match against the Nuffield Department of Medicine was always a tense affair. With his colleague Sir Roy Calne, also an excellent tennis player and Professor of Surgery at the University of Cambridge, the annual cricket and tennis matches were also much anticipated.
Peter was a guest on BBC Radio 4 Desert Island Discs in 2002.
He was elected as Fellow of the Royal Society in 1994, was a foundation fellow of the Academy of Medical Sciences in 1998 and President of the Royal College of Surgeons (RCS) England 2001-2004. As Chairman of the RCS Research Board, he championed the Research Fellowship Scheme to facilitate the training of surgeon scientists. He was awarded the Lister Prize for his contributions to surgical science in 2006.
Peter was knighted by Queen Elizabeth II in 1996 for services to Medicine and made a Companion of the Order of Australia in 2004. He retired from the Nuffield chair in 2001, continuing to be active in the field developing The Transplant Library designed access to high quality, evidence-based information on all of aspects of solid organ transplantation.
Peter will be sadly missed by friends and colleagues in many parts of the world.
He is survived by his wife Joce and their children and families.
Professor Sir Peter Morris AC FRS - April 17, 1934 to October 29, 2022

Sir Peter Morris
Medawar Prize Laureate (2006)

Medawar Price 2006
Introduction of Sir Peter John Morris
Peter Morris was born in Horsham, Victoria, Australia where he enjoyed a happy, healthy, confident boyhood. He studied medicine at the University of Melbourne in the 1950s, interrupted by the obligatory tour of national service. He describes his medical school years as one of the happiest times of his life. Interestingly, he recalls being blissfully unaware of the developments occurring in transplantation at this time elsewhere in the world. Immunology teaching at the University of Melbourne was quite rudimentary, consisting of only three lectures by Sir MacFarlane Burnett who interestingly later shared the Nobel Prize in Medicine in 1960 with Sir Peter Medawar for theories of immunological tolerance.
The early surgical training of Peter Morris was at the Hammersmith Hospital in London. There he was exposed to some clinical transplantation in the renal transplant program of James Dempster and Ralph Shackman, but his interest in transplantation remained unstimulated. In 1964, Morris was offered additional surgical training at the Massachusetts General Hospital (MGH) through the efforts of Dr. Claude Welch and in the following year joined the laboratory of Dr. John Burke to study surgical infection and inflammation. At this time the new Chief of Surgery, Paul S. Russell, had initiated an active renal transplant program at the MGH with encouraging results with living related kidney transplants. Russell also established an active transplantation/immunology research laboratory focused on analysis of histocompatibility. Morris’ regular interaction with research fellows in Russell’s laboratory, many of whom were from England, nurtured his early interest in histocompatibility, which in turn led to a shift in his research emphasis from infection and inflammation to transplantation. With the help and intercession of Paul Russell, Morris was introduced to and developed strong interactions with Bernard Amos, Jan van Rood, and Paul Terasaki, the early histocompatibility pioneers.
Prior to his return to the University of Melbourne, Morris spent six months establishing the tissue typing laboratory at the Medical College of Virginia with David Hume, who had established one of the major transplant units in the United States. During this period he established a long-lasting collaborative friendship with Paul Terasaki. Together they demonstrated for the first time in humans using stored sera of Hume’s patients that cytotoxic antibodies were present in the sera of patients after transplantation, particularly if they had rejected a transplanted kidney. In addition, with Mel Williams and others, Morris showed that in the presence of recipient cytotoxic antidonor antibodies, immediate rejection of the kidney would occur.
In 1967, Peter Morris returned to the University of Melbourne and the Department of Surgery at the Royal Melbourne Hospital to establish the first histocompatibility laboratory in Australia. He was able to show the first correlation between cadaver graft outcome and HLA typing. At this time, he was interested in all aspects of HLA, not just its application to transplantation. He studied the possible association of HLA with susceptibility to different diseases, eventually showing a reasonably strong association of HLA with Hodgkin’s disease, with chronic active hepatitis and with pancreas islet antibodies in diabetes. He also pursued anthropological studies of HLA in various population groups of Southeast Asia, Fiji, and New Guinea, and in Australian aborigines, which demonstrated—among other things—the extraordinary limited polymorphism of the HLA system in certain populations.
In 1974, at the tender age of 39, Peter Morris was appointed Nuffield Professor of Surgery and Chairman of the Department at Oxford University. The department flourished under his leadership. He established the Oxford Transplant Center, which introduced a number of clinical trials in transplantation—a relatively rare undertaking in these early days. Among these was the first demonstration in 1978 of the salutary effect of matching for HLA-DR alone in cadaveric renal transplantation . In addition, Morris and colleagues showed that many patients can be transplanted in the presence of positive crossmatches when the antibodies involved are not directed against HLA. In addition to a vigorous clinical transplantation program, Morris also established a transplantation biology research laboratory in which he nurtured strong collaboration and cooperation with basic scientists. A critical part of the Oxford laboratory effort involved a Ph.D. program in which visiting research fellows—many of whom were clinicians—came to the Oxford transplantation laboratory for postgraduate research training. The Oxford transplantation biology research program has grown steadily to involve multiple areas of basic and translational research in experimental transplantation immunobiology. Over the years, a host of associates, graduate students, and research fellows from all over the world worked in the Oxford laboratory. These colleagues and graduates are the physician- and surgeon-scientists who currently hold leadership positions in transplantation throughout the world and who continue to make major contributions today—a legacy of which Sir Peter should be enormously proud.
Dr. Morris’ bibliography contains in excess of 800 scientific papers and scholarly works. In addition to his studies on HLA and clinical transplantation he has made seminal contributions in experimental studies on: 1) the role of blood transfusions and passive enhancement in experimental renal and islet cell allografts, 2) the migration of dendritic leukocytes from allografts to initiate rejection, 3) use of nondepleting monoclonal anti-CD4 antibodies to modify rejection, 4) analysis and role of T regulatory cells and altered cytokine pathways in tolerance, and 5) induction of tolerance by retroviral transfer of donor major histocompatibility complex antigens into recipient bone marrow cells.
The impact of Sir Peter Morris on the field of transplantation and the respect accorded him by his colleagues are reflected in his awards and achievements. He has been elected to leadership positions of numerous academic and professional societies including as Chairman of the British Transplantation Society (1976–77) and as President of The Transplantation Society (1984–86), the British Society of Histocompatibility and Immunogenetics (1993–95), the European Surgical Association (1996–98), the International Surgical Society/Société de Chirurgie (2001–03), and most recently, The Royal College of Surgeons of England (2001–04). He has had the honor to deliver over 40 distinguished lectureships, including the Lister Oration and the Hunterian Oration of the Royal College of Surgeons, England. He has also received numerous awards in the form of prizes, named professorships, honorary fellowships, and honorary degrees including most noteworthy Fellowship in the Royal Society (1994), the Lister Medal (1997), and the Hunterian Medal (2005). In 1996, he received Knighthood for Services to Medicine (Fig. 4). In addition, he has been listed as one of the world’s most cited authors in clinical medicine by the Information Sciences Institute.
Finally, and most importantly, in addition to all these accomplishments Peter Morris is a grand human being—a loving husband, proud father, and devoted grandfather to his family and a cherished friend to his colleagues. Years ago I stated at one of these congresses that transplantation was fortunate to have so many gifted and dynamic people to lead this young field to future greatness. I likened transplantation to a sky full of shining stars. It is my pleasure to present one of our most shining stars, perhaps the shiniest, Peter Morris, as a 2006 Medawar Prize winner.
Monaco, Anthony P.
Transplantation: December 27, 2006 - Volume 82 - Issue 12 - p 1587-1589
Medawar Prize Acceptance Speech
Highlighted Articles
Highlighted Videos
Interview with Sir Peter Morris
Sir Peter Morris message to the Texas Transplantation Society
Pioneers of transplantation Peter Morris
Contact
Address
The Transplantation Society
International Headquarters
740 Notre-Dame Ouest
Suite 1245
Montréal, QC, H3C 3X6
Canada
Используйте Вавада казино для игры с бонусом — активируйте промокод и начните выигрывать уже сегодня!

