In the Northern Hemisphere we are in the middle of the Winter season, a season filled with holidays. There may be close to 20 holidays during this season. Some are celebrated worldwide and some regionally.
The reason I bring this up is that many of these holidays are celebrated indoors, and we are still facing the COVID-19 pandemic. As I am writing this letter, a new variant, Omicron, has been identified in 18 countries and is likely present in most others. However, it is too early to tell whether this variant is more transmissible than other variants, including Delta, or if it will cause more severe disease and whether the current vaccines and treatments will be less effective.
Do we need to be concerned? Yes, but I would say, very little! What we know is that the risk of transmission of COVID-19 is diminished if we follow all the precautions with which we have become accustomed: social distancing, mask-wearing, hand washing, and immunization.
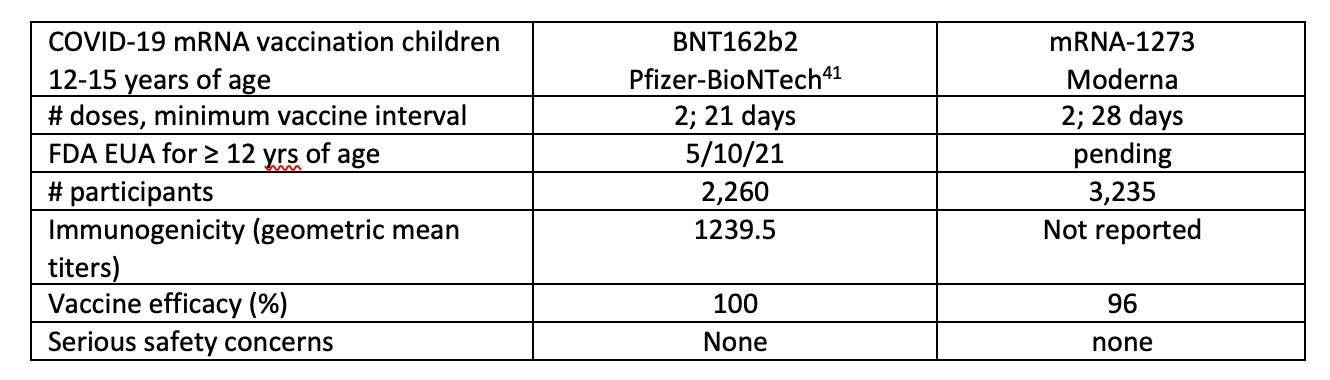
Vaccines remain the most effective tool against COVID-19. We do need to protect our immunosuppressed children since most around the world are not or only partially vaccinated. I urge the manufacturers of the COVID-19 vaccine to make it available, particularly to low-resource countries. These countries remain vulnerable to continued disease and viral replication with almost no access to vaccines! The research for efficacy and safety in young children, particularly in immunocompromised kids, must be expedited, and I do hope pediatric transplant recipients will get priority when available.
Now, looking back, IPTA did have a very busy year. Here are some of the highlights:
- IPTA Fellows & Allied Health Symposium, October 2021
- SMARTER (Social Media for International Pediatric Transplantation) Initiative pioneered by the IPTA Education Committee (content has included a podcast, a Journal Club, and 2 webinars, more to come!)
- Launch of IPTA 2021 and 2022 Outreach Programs
- Endorsement of Declaration of Istanbul and development of Pediatric Priority position statement
- IPTA Allied Health & Nursing Professionals Committee webinar series
- Continuation of planning for IPTA 2022 Congress
In my humble opinion, I feel that we are coming out of this pandemic. I do wish the IPTA membership, and staff a Holiday Season filled with optimism, joy and love!
Yours faithfully,
Carlos O. Esquivel
IPTA President

From all of us at IPTA, Happy Holidays, and we look forward to a healthy and prosperous 2022!
Past Issues
IPTA Newsletters
- IPTA Newsletter - February 2026
- IPTA Newsletter - December 2025
- IPTA Newsletter - October 2025
- IPTA Newsletter - June 2025
- IPTA Newsletter - March 2025
- IPTA Newsletter - December 2024
- IPTA Newsletter - October 2024
- IPTA Newsletter - May 2024
- IPTA Newsletter - February 2024
- IPTA Newsletter - November 2023
- IPTA Newsletter - September 2023
- IPTA Newsletter - May 2023
- IPTA Newsletter - March 2023
- IPTA Newsletter - December 2022
- IPTA Newsletter - October 2022
- IPTA Newsletter - July 2022
- IPTA Newsletter - May 2022
- IPTA Newsletter - December 2021
- IPTA Newsletter - October 2021
- IPTA Newsletter - June 2021
- IPTA Newsletter - October 2020
- IPTA Newsletter - June 2020
- IPTA Newsletter - March 2020
- IPTA Newsletter - December 2019
- IPTA Newsletter - September 2019
- IPTA Newsletter - July 2019
- IPTA Newsletter - April 2019
- IPTA Newsletter - December 2018
- IPTA Newsletter - September 2018
- IPTA Newsletter - June 2018
- IPTA Newsletter - March 2018
- IPTA Newsletter - December 2017
- IPTA Newsletter - September 2017
- IPTA Newsletter - December 2016
- IPTA Newsletter - September 2016
Social
Contact
Address
International Society of Uterus Transplantation
c/o The Transplantation Society
740 Notre-Dame Ouest
Suite 1245
Montréal, QC, H3C 3X6
Canada